Thanks to the recent developments in transplant procedures, an increasing number of patients with acute myeloid leukemia (AML) with a poor Karnofsky Performance Status (KPS) score are currently offered an allogeneic hematopoietic stem cell transplantation (allo-HCT). Nevertheless, little data is available about outcome of this fragile population.
We report here the results of a retrospective study designed to evaluate outcome of patients with AML undergoing allo-HCT with KPS score ≤80%. The analysis included patients with AML aged ≥18 years, undergoing allo-HCT in first remission between 2000 and 2018, with a KPS score at the time of transplant between 50% and 80%. Patients who received manipulated grafts or had incomplete data about cytogenetics were excluded. Conditioning intensity was defined according to EBMT definitions.
A total of 2,963 patients were identified. Median age at transplant was 55 years (18-77 years). Median year of transplant was 2014. The KPS score was =80% in 85% of the patients and <80% in 15% of the patients. Cytogenetic risk was good, intermediate or poor in 6%, 68% and 26% of the patients, respectively. Donor type was sibling (MSD), matched (10/10 UD), mismatched (9/10 UD) unrelated, haploidentical (haplo) or cord blood (CB) in 47%, 35%, 8%, 6% and 4% of patients, respectively. Conditioning was myeloablative (MAC) or reduced-intensity (RIC) in 42% and 58% of patients. Stem cell source was PBSC or BM in 84% and 14% of the patients. Anti-thymocyte globulin (ATG) was administered to 55% of the patients.
Cumulative incidence of grade II-IV and III-IV acute GVHD (aGvHD) was 26% and 8%, respectively. The 2-year cumulative incidence of chronic GVHD (cGvHD) and severe cGVHD was 38% and 18%. Non-relapse mortality (NRM) and relapse incidence (RI) at 2 years were 19% and 27%, respectively. Notably, in the subgroup of patients with KPS <80% NRM rate was as high as 27%. At 2 years, leukemia-free survival (LFS), overall survival (OS) and GVHD-free, relapse-free survival (GRFS) rates were 54%, 59% and 41%, respectively.
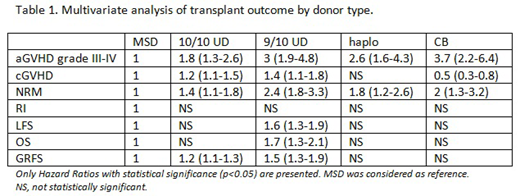
On multivariate analysis, transplant from a MSD was associated with a reduced risk of aGvHD (10/10 UD HR 1.8, 9/10 UD HR 2.4, haplo HR 1.9, CB HR 3.4, p<10-4, MSD as reference) and NRM (10/10 UD HR 1.4, 9/10 UD HR 2.4, haplo HR 1.8, CB HR 2, p<10-3, MSD as reference) as compared to all other donor types (Table 1). Transplant from 10/10 UD was associated with lower GRFS (HR 1.2, p=0.03), while 9/10 UD predicted inferior LFS, OS and GRFS (HR 1.6, 1.7, and 1.5, respectively, p<0.001) as compared to MSD. Patients with KPS score of 80% had significantly lower NRM and improved survival as compared to patients with KPS score <80% (NRM: HR 0.6, p<10-4; OS: HR 0.7, p<10-4). Other factors independently associated with improved OS were younger age, female sex, good or intermediate risk cytogenetics and de-novo AML. Notably, administration of ATG was associated with reduced risk of developing grade II-IV aGVHD (HR 0.7, p<10-4), cGVHD (HR 0.6, p<10-4), severe cGVHD (HR 0.5, p<10-4) and predicted improved GRFS (HR 0.8, p<0.01).
In order to compare outcome following MAC and RIC conditioning the analysis was restricted to patients receiving transplant from MSD or UD. Patients with a KPS score =80% or <80% were analyzed separately. In the group of patients with a KPS score of 80%, a RIC regimen was associated with higher RI (HR 1.4, p<0.01), higher incidence of severe cGVHD (HR 1.6, p<0.001), and inferior GRFS (HR 1.3, p<0.001) as compared to MAC. NRM was not significantly different following RIC or MAC in this population. In contrast, in patients with a KPS score <80%, RIC was associated with lower NRM (HR 0.3, p<0.0001) and better LFS (HR 0.6, p<0.01), OS (HR 0.5, p<0.0001) and GRFS (HR 0.6, p<0.01) as compared to MAC.
In conclusion, allo-HCT is feasible in patients with acute myeloid leukemia in first remission and KPS score <80%, with acceptable NRM and survival rates. As for the conditioning regimen, in patients with a KPS score of 80% a MAC regimen was associated with lower relapse rate, similar NRM and better GRFS as compared to RIC, while in patients with a KPS score lower than 80% RIC was associated with reduced NRM and improved OS as compared to MAC. In addition, transplant from a MSD predicted a reduced risk of NRM and aGVHD as compared to other donor types. Notably, 9/10 UD was associated with significantly inferior survival as compared to MSD. Finally, administration of ATG correlated with reduced acute and chronic GVHD and improved GRFS.
Labopin:Jazz Pharmaceuticals: Honoraria. Kröger:Sanofi-Aventis: Research Funding; Celgene: Honoraria, Research Funding; DKMS: Research Funding; JAZZ: Honoraria; Medac: Honoraria; Neovii: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Riemser: Research Funding. Socie:Alexion: Consultancy. Blaise:Pierre Fabre medicaments: Honoraria; Jazz Pharmaceuticals: Honoraria; Sanofi: Honoraria; Molmed: Consultancy, Honoraria. Byrne:Ariad/Incyte: Honoraria, Speakers Bureau. Esteve:Astellas: Consultancy, Speakers Bureau; Novartis: Consultancy, Research Funding, Speakers Bureau; Celgene: Consultancy, Speakers Bureau; Amgen: Consultancy; Daiichi Sankyo: Consultancy; Jazz Pharmaceuticals: Consultancy; Roche: Consultancy; Pfizer: Consultancy. Mohty:Jazz Pharmaceuticals: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal