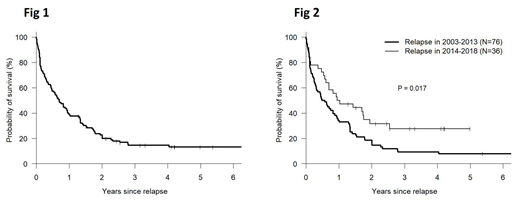
Relapse of leukemia (RL) is the most common cause of treatment failure following allogeneic hematopoietic cell transplantation (alloHCT) in patients with AML. Historically, patients who suffer RL following alloHCT have had a dismal prognosis. A number of therapeutic options have recently become available for relapsed/refractory AML, including some that are associated with limited toxicity and may be well tolerated in the post-alloHCT setting. These therapies, and advances in supportive care have the potential to prolong survival of recently transplanted patients who suffer RL post post-alloHCT compared to prior cohorts. We hypothesized that patients suffering RL post-alloHCT within the last 5 years will have improved post-relapse survival compared to patients experiencing RL before this period. In order to test this hypothesis, we analyzed 309 patients who underwent a first allo-HCT for AML between Jan 2002 and Dec 2016 at our center and identified 112 patients (36%) who suffered RL post-alloHCT. Data were extracted from our institutional BMT database where they had been prospectively entered. Patient characteristics of those who experienced RL were: median age 53 (19-74); male - 51%; race- white-86%, black 12%, Asian -2%; donor-MRD 33%, MUD 41%, Haplo 26%; graft source - PBSC 86%, BM 11%, CBU 2%, PBSC+BM 1%; regimen intensity - MAC 61%, NST/RIC 39%%; DRI - intermediate 46%, high 50%, v. high 5%; HCT-CI 0-2 (58%), >3 (42%); KPS > 90 (39%) <90 (61%), CMV - pos 70%, neg 29%, year of relapse -2003-2013 (68%), 2014-2018 (32%). Median time from alloHCT to relapse was 170 days (25-1106). Median follow-up of surviving patients was 50 months (15-143). DLI: A first DLI was administered to 19 patients at a median of 41 days post relapse. The corresponding number of patients receiving 2nd, 3rd and 4th DLI were 12, 6 and 2 patients given at a median of 62, 48 and 38 days following the prior DLI. A second alloHCT post RL was performed in 33 patients (29%) at a median of 85 days (22-772d) post relapse using the same donor as the first allo-HCT in 45% and a different donor in 55%. The second transplant was from a MRD, MUD and Haplo donor in 10, 11 and 12 patients respectively. Estimates of post-relapse survival at 1, 2 and 3 years following relapse for all patients are 39%, 23% and 15% (Fig 1). For patients whose AML relapsed between 2003-2013, and 2014-2018 estimated 1, 2, and 3 year survival rates following relapse were 34%, 18% and 9% vs 50%, 32% and 28% respectively (p=0.017, Fig 2). A multivariable Cox model was developed for post-relapse survival considering the following variables: at relapse, gender, race, time from transplant to relapse, donor type, graft source, regimen intensity DRI, HCT-CI, KPS, CMV status, DLI post relapse , second alloHCT post relapse, year of relapse. Second alloHCT post-relapse was tested as a time-dependent covariate. Variables were selected if the p value was less than 0.05. Proportionality was tested for selected variables and all variables passed the test. On multivariable analysis, survival was significantly better for patients who relapsed in 2014-2018 vs patients relapsing in prior years (2003-2013) - HR 0.55. p=0.018. Other variables associated with post-relapse survival were time from BMT to relapse >250 d vs <100 d - HR 0.55, p=0.025 and haplo donor vs MRD for first alloHCT- HR 2.41, p=0.002. The use of DLI or the occurrence of a second alloHCT post-relapse tested as a time-dependent co-variate were not significantly associated with survival in this analysis. These data suggest that survival for AML patients who suffer relapse of malignancy following alloHCT has improved in recent cohorts when compared to historic controls. Approximately one-half and one-third of the patients are now estimated to live 1 and 2 years following relapse and prolonged survival is possible in some cases. The impact of specific interventions that help promote survival following relapse should be further studied
Solh:ADC Therapeutics: Research Funding; Celgene: Speakers Bureau; Amgen: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal