Introduction: Recent data emerges that transplantation with reduced intensity conditioning (RIC) seems to be effective as myeloablative conditioning (MAC). However, relapse is a major concern with RIC, and identification of patients at equivalent probability of relapse irrespective of conditioning intensity is needed.
Method: A total of 567 AML patients underwent allogeneic hematopoietic stem cell transplantation (HSCT) betwene June 2012 and Jan 2018. For this study, we selected 287 patients who fulfilled i) intermediate or poor risk group by NCCN (2017.Version 3), ii) CR or CRi at HSCT, iii) received either MAC (BuCy or CyTBI) or RIC (FluBu2TBI400) peripheral blood stem cell transplant from 8/8 matched sibling donor (MSD) or matched unrelated donor (MUD), and iv) having bone marrow Wilms tumor gene 1 (WT1) expression results before transplant. The association between conditioning intensity, WT1 level at HSCT and post-transplant clinical outcomes involving overall survival (OS), disease free survival (DFS), cumulative incidence of relapse (CIR) and nonrelapse mortality (NRM) were evaluated first. And then we attempted to compare post-tranpslant outcomes between MAC and RIC groups in pre-transplant WT1low patients only.
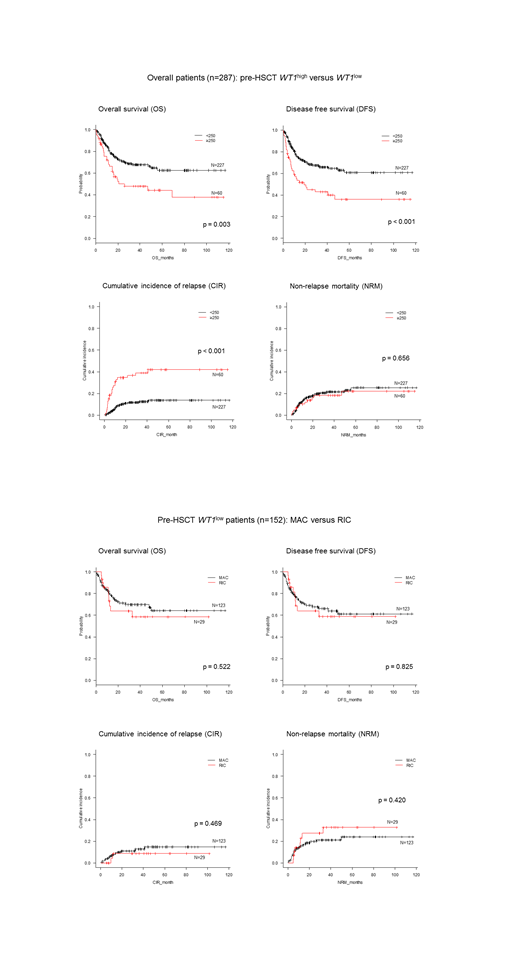
Results: Among the total 287 patients, 232 (80.8%) and 55 (19.2%) patients received MAC and RIC transplant. The median WT1 gene expression level at diagnosis (assessable in 255 patients) was 2310.0 copies/104ABL. When ≥ 250 copies/104ABL were classified as high expression of WT1 (WT1high), 77.3% (n=197) showed WT1high at AML diagnosis. In multivariate analysis, older age and WT1high before HSCT were designated as independent prognostic factor for inferior OS, DFS and higher CIR, and NCCN risk group at diagnosis was significantly associated with incidence of relapse; whereas, conditioning intensity or WT1 level at diagnosis were not prognostic for post transplant outcomes. After excluding patients without available information on initial WT1 level (n=32), whose WT1 levels were not overexpressed at diagnosis (n=58), and whose WT1 level ≥ 250 copies before transplant (n=45), we finally selected 152 pre-trasnplant WT1low patients for further analysis. Older age was still a significant independent factor for poor OS, DFS and higher NRM, whereas NCCN risk stratification at diagnosis was no longer prognostic for post-transplant outcomes in pre-trasnplant WT1low patients only. There was no significant difference in these outcomes between MAC (n=123) and RIC (n=29) patients, and pre-HSCT WT1 level as continuous variable remain significant for predicting relapse even if the level was below 250 copies.
Conclusion: Post-transplant survival or relapse did not differ by conditioning intensity in AML CR1 patients whose WT1 level was below 250 copies per 104 ABL at transplant.
Kim:BMS: Research Funding; Pfizer: Research Funding; Il-Yang co.: Research Funding; Novartis: Research Funding; Takeda: Research Funding. Lee:Alexion: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Achillion: Research Funding. Kim:Celgene: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Hanmi: Consultancy, Honoraria; AGP: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; SL VaxiGen: Consultancy, Honoraria; Novartis: Consultancy; Amgen: Honoraria; Chugai: Honoraria; Yuhan: Honoraria; Sanofi-Genzyme: Honoraria, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Handok: Honoraria; Janssen: Honoraria; Daiichi Sankyo: Honoraria, Membership on an entity's Board of Directors or advisory committees; Otsuka: Honoraria; BL & H: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal