Background: Smoldering multiple myeloma (SM) is a heterogenous clinical entity with a variable rate of progression to symptomatic multiple myeloma (MM). Identification of demographic characteristics and outcomes of SM patients have been hampered by the lack of specific ICD code for SM. Here, we analyzed the National Cancer Database (NCDB) for this purpose, which covers >70% of cancer patients in the U.S.
Methods: We reviewed patients in the NCDB who were diagnosed with MM between 2010 and 2014. Patients who did not receive any treatment within 3 months after the diagnosis and still alive were considered to have had SM (Ravindran et al. Blood Cancer J. 2016). Initiation of systemic treatment was considered as a surrogate of progression to symptomatic MM. Overall survival (OS) of SM patients was calculated from initiation of systemic treatment after they progressed to MM, estimated by the Kaplan-Meier method, and compared with the log-rank test. Cumulative incidence of progression from SM to MM was calculated with death as a competing risk and compared with the Gray's test. Multivariable Cox and logistic regression analysis were performed to identify independent predictors of OS and progression to MM, respectively.
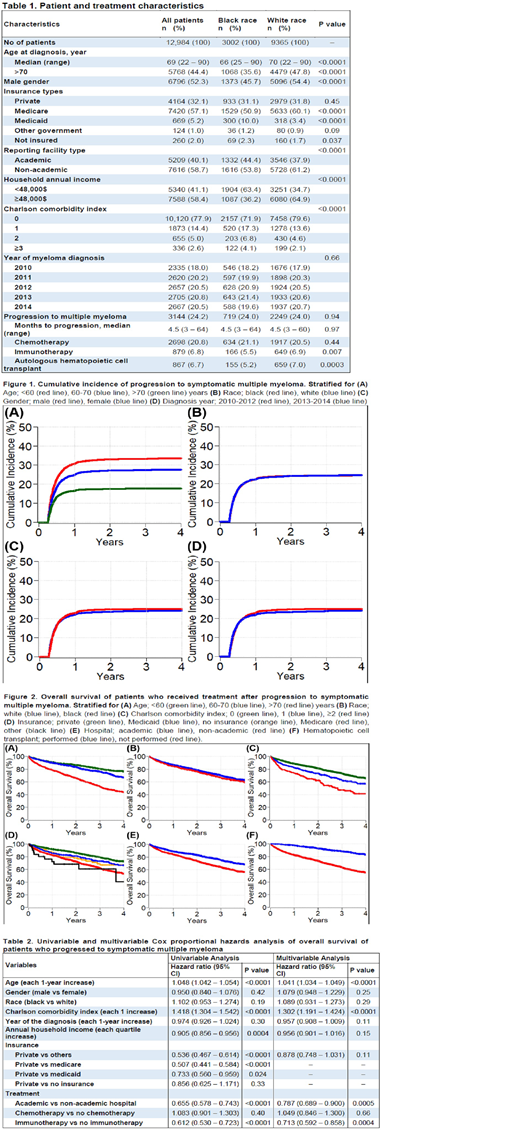
Results: We reviewed 68,234 patients and identified 12,984 patients with SM. Among SM patients, 3002 (23%) were black, 6796 (52%) were male, and median age at diagnosis was 69 years (range: 22 - 90). SM patients' insurance types were private for 4164 (32%), Medicare for 7420 (57%), Medicaid for 669 (5%), and 260 (2%) were uninsured. Majority of the cases were reported from non-academic hospitals (59%). Patient and treatment characteristics are summarized in Table 1. SM was diagnosed in black patients a median of 4 years younger than in white patients (median age 66 vs 70 years, p<0.0001). Charlson comorbidity index was 2 or more for 325 (11%) black and 629 (7%) white patients (p<0.0001). Median annual household income of white patients was higher than black patients (p<0.0001). Median time to progression from SM to MM was 4.5 months (range: 3 - 64). Progression to MM was seen in 3144 (24%) patients during median follow-up of 39 months. All SM patients received chemo- or immunotherapy after progression and 867 (7%) underwent hematopoietic cell transplant.
Four-year cumulative incidence of progression to MM for SM patients at ages of <60 vs 60-70 and >70 years was 34% (95% CI: 32 - 35) vs 28% (95% CI: 26 - 29, p<0.0001) and 18% (95% CI: 17 - 19, p<0.0001), respectively (Figure 1A). Four-year cumulative incidence of progression to MM for patients of black and white race was 24.5% (95% CI: 23 - 26) and 24.4% (95% CI: 24 - 25), respectively (p=0.99) (Figure 1B). Four-year cumulative incidence of progression to MM for patients who were diagnosed between 2010-2012 and 2013-2014 was 25% (95% CI: 24 - 26) and 24% (95% CI: 23 - 25), respectively (p=0.17) (Figure 1D). On multivariable analysis, each 10-year decrease in age (OR 1.06, 95% CI: 1.05 - 1.06, p<0.0001), white vs black race (OR 1.02, 95% CI: 1.00 - 1.04, p=0.027), and each 1-year decrease in diagnosis year (OR 1.01, 95% CI: 1.00 - 1.01, p=0.015) were associated with progression to MM, however male vs female gender (OR 1.01, 95% CI: 0.99 - 1.02, p=0.26) was not statistically significant.
Four-year OS of SM patients after progression and MM patients without known preceding SM who received treatment were 63% (95% CI: 61 - 65) and 54% (95% CI: 54 - 55), respectively (p<0.0001). Figure 2 shows OS of the patients with SM in several subgroups. Four-year OS of SM patients after progression to MM at ages of >70 vs 60-70 and <60 years were 44% (95% CI: 40 - 48) vs 67% (95% CI: 63 - 71, p<0.0001) and 76% (95% CI: 73 - 80, p<0.0001), respectively (Figure 2A). On multivariable analysis, each 1-year increase in age (HR 1.04, 95% CI: 1.03 - 1.05, p<0.0001), each 1 increase in Charlson comorbidity score (HR 1.30, 95% CI: 1.19 - 1.42, p<0.0001), academic vs non-academic hospital (HR 0.79, 95% CI: 0.69 - 0.90, p=0.0005), and immunotherapy vs no immunotherapy (HR 0.71, 95% CI: 0.59 - 0.86, p=0.0004) were statistically significant predictors of OS (Table 2).
Conclusion: Taken together, our result shows higher rate of MM progression in younger SMM patients than old ones as well as earlier age of SMM diagnosis in Blacks. Also, this study highlights the importance of known SMM stage before MM in prolonging survival which can be indicative of benefit from screening programs.
Metheny:Incyte: Speakers Bureau; Takeda: Speakers Bureau. Malek:Celgene: Consultancy; Takeda: Consultancy; Sanofi: Consultancy; Medpacto: Research Funding; Janssen: Speakers Bureau; Amgen: Speakers Bureau; Adaptive: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal