Introduction
Diagnosis and follow-up monitoring of Multiple Myeloma (MM) requires documentation of (clonal) plasma cells using morphological bone marrow assessment and other ancillary studies including CD138 immunohistochemistry (IHC), flow cytometry (FC), and myeloma-specific fluorescence in situ hybridization (FISH). While IHC and FC have traditionally been shown to be the more sensitive methods for the assessment of residual disease, the detection rates of FISH have markedly increased with the recent use of magnetic cell sorting for CD138 cell enrichment. We, therefore, aimed to revisit the clinical utility of these ancillary studies in the diagnosis and follow-up of MM.
Methods
We retrospectively reviewed the reports of bone marrow biopsy specimens received for the initial diagnosis or follow-up assessment of MM from October 2015 to January 2019. All cases that had both FC and FISH performed were included in the analysis. Patient demographics, treatment history and the results of bone marrow evaluation were recorded.
Results
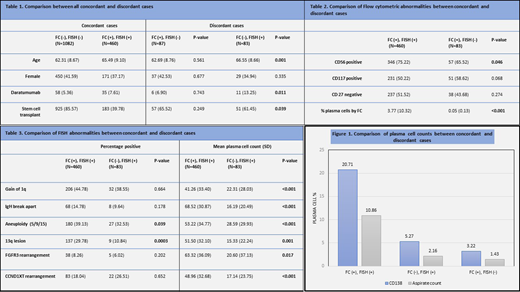
During the study period, we evaluated a total of 1,712 biopsy specimens from 464 MM patients (mean±SD age: 64.0±9.4 years; females 41.4%). Of these, 87 cases were submitted for initial diagnosis and 1,625 cases had already established MM and were being evaluated for post-treatment residual disease. For both initial diagnosis and follow-up cases, CD138+ IHC demonstrated highest plasma cell burden (mean: 49.1% and 4.6%, respectively) followed by morphological aspirate count (mean: 29.6% and 2.3%, respectively) and FC (mean: 10.9% and 1.8%, respectively). Both FC and FISH had comparable detection rates at the time of initial diagnosis (95.4% versus 97.7%, respectively) and for follow-up cases (28.6% versus 28.2%, respectively). The FC and FISH results were concordant in 97.7% of the initial diagnosis cases and 89.7% of follow-up cases. Discordant cases with positive FISH results and negative FC results included 2 (2.3%) initial diagnosis cases and 81 (5.0%) follow-up cases whereas those with negative FISH and positive FC results included 87 (5.3%) follow-up cases.
In comparison with all concordant cases, the FISH positive, FC negative discordant cases were older in age, more likely to have received treatment with Daratumumab, and less likely to have received stem cell transplantation (p <0.05) (Table 1). When compared to the FC and FISH positive concordant cases; both discordant groups had significantly lower plasma cell counts detected by the aspirate smear and CD138+ IHC (Figure 1). Among all FC positive cases, the discordant cases had lower FC detected plasma cell counts and were less likely to have aberrant CD56 expression as compared to the concordant cases (p <0.05) (Table 2). Finally, among all FISH positive cases, the discordant cases were less likely to have 13q lesion and aneuploidy of chromosomes 5, 9, and 15 (p <0.05) as compared to the concordant cases. Also, between these groups, the percentage of plasma cells with individual FISH aberrations was significantly lower among the discordant cases (Table 3).
Conclusion
Overall, FISH (with magnetic cell sorting) and FC have comparable detection rates at the initial diagnosis and follow-up assessment. Approximately 10% of the follow-up cases have discordant FISH and FC results where residual disease is detected by only one of these modalities. Also, the discordant cases have significantly lower plasma cell counts as compared to the FC and FISH positive concordant cases. Therefore, this study suggests that both FC and FISH are useful for the follow-up monitoring of MM, especially in the cases with low plasma cell burden. Finally, the higher frequency of Daratumumab treatment in FISH positive, FC negative discordant cases might suggest Daratumumab's potential interference with the residual disease detection by FC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal