Introduction:
Duvelisib (DUV), an oral inhibitor of PI3K-δ/γ, and venetoclax (VEN), an oral inhibitor of BCL-2, are both approved for relapsed/refractory (R/R) CLL. We previously found that PI3K-δ inhibition sensitizes CLL cells to ex vivo BCL-2 inhibition (Davids et al., Blood, 2012). We hypothesized that DUV plus VEN would lead to deep remissions that allow for an all oral, time-limited therapy. Here, we report for the first time on a phase I study of DUV plus VEN for patients (pts) with R/R CLL/SLL.
Methods:
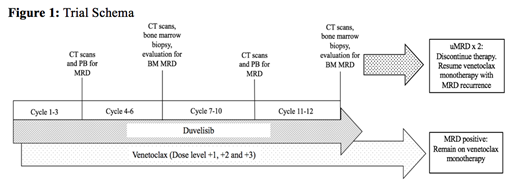
This is an investigator-initiated phase I trial with primary endpoints: DLTs, MTD, and RP2D of VEN plus DUV in pts with R/R CLL/SLL. Secondary endpoints: PK, preliminary efficacy. Pts are treated as per Figure 1, with a 7-day lead-in of DUV 25 mg BID. On day 8, DUV was continued and VEN initiated at 10 mg QD, with weekly ramp-up to 20/50/100 (dose level 1), 200 mg (dose level 2), and 400 mg (dose level 3). The last 3 pts initiated VEN at 20 mg. A 3+3 design was used, and the DLT observation period was the first cycle. Eligibility criteria: ≥1 prior therapy, requiring therapy by 2008 iwCLL criteria, ECOG PS ≤2, adequate hematologic and organ function, no prior VEN or DUV. CTCAE v5 and 2008 iwCLL were used to evaluate toxicity and efficacy. PK testing was performed at each VEN dose escalation and just prior to cycle 2. MRD was assessed by 8-color flow at a sensitivity of 10-4 (Mayo Laboratories) in the peripheral blood (PB) and bone marrow (BM).
Results:
As of July 12, 2019, 12 pts were evaluable. Median age 69 yrs (range 50 to 78). Del(17p): 3/12 (25%), del(11q): 1/12 (8%), unmutated IGHV: 12/12 (100%), mutation in NOTCH1: 7/12 (58%) and TP53: 5/12 (42%) pts. Median prior treatments: 3 (range 1-6), including 2 pts relapsed after alloHCT. Ten pts had prior BTKi, including 3 who progressed on therapy. No DLTs were observed, and the RP2D of VEN in combination with DUV was the approved dose of 400 mg. Most pts had baseline cytopenias, with a median ANC of 3 (range 1.19-7.78), Hgb 7 (range 7.6-13.5), PLT 43 (range 21-221). Heme toxicities were common and included: neutropenia (100%, 83% ≥ gr3), anemia (100%, 33% ≥ gr3), and thrombocytopenia (75%, 8% ≥ gr3). Nine pts required G-CSF support. All grade non-heme tox in >25% of pts: fatigue (92%, all gr1/2), hyperglycemia (100%, 25% gr1, 58% gr2, 17% gr3), hypocalcemia (100%, 50% ≥ gr3), hypophosphatemia (67%, 25% ≥ gr3), elevated alk phos (58%, all gr1/2), elevated AST (58%, all gr1/2), hypokalemia (50%, 17% ≥ gr3), hypomagnesemia (50%, all gr1/2), rash (50%, 8% ≥ gr3), diarrhea (42%, 8% ≥ gr3), and hyponatremia (42%, 8% ≥ gr3). SAEs: gr3 amylase/lipase, and gr3 febrile neutropenia (n=1 each). No laboratory or clinical tumor lysis syndrome (TLS) was observed per Cairo-Bishop criteria. One pt with medium TLS risk who initiated VEN at 20 mg had an increase in LDH prompting a brief VEN hold; a second pt with medium TLS risk had an early rise in K rapidly responsive to intervention and later LDH increase prompting a brief VEN hold. Five patients required DUV holds for asymptomatic elevation in amylase and/or lipase (n=4), rash (n=2), bronchitis (n=1), or diarrhea (n=1). Four pts required steroids for toxicity management. PK analyses demonstrated that VEN exposure increased with increasing doses in the presence of DUV. After receiving 25 mg DUV BID, 4h VEN plasma concentrations following 200 mg and 400 mg VEN were 1,803±819 ng/mL and 2,363±1134 ng/mL, respectively. These VEN concentrations are similar to values in the literature, suggesting no significant drug/drug interaction.
At data cutoff, median number of treatment cycles was 6 (range 1-9), and the first 9 pts were evaluable for response (6 had 2 response assessments). Eight of the 9 pts achieved response, with 3 CRs and 5 PRs. Two pts had undetectable MRD (uMRD) in PB and BM (including 1 pt with CR and 1 pt with minimal nodes with SD). One pt with a CR was PB-uMRD only. Three pts have discontinued (1 electively moved to alloHCT, 2 with PD (including 1 ibrutinib progressor who developed Richter's Syndrome (RS)).
Conclusions:
DUV plus VEN is feasible in pts with R/R CLL/SLL, with no DLTs observed, and a RP2D of VEN 400 mg with DUV 25 mg BID. Although high rates of neutropenia were observed, infections were infrequent. Early efficacy data for this 1-year time-limited, all oral regimen are promising, with CRs and uMRD already observed despite short follow-up. Updated results will be presented at the meeting, and a phase II trial, which includes a cohort for RS, will further evaluate efficacy.
Montegaard:Pharmacyclics: Consultancy; Janssen: Consultancy. Soumerai:AbbVie: Consultancy; Verastem: Consultancy; BostonGene: Research Funding; Genentech/Roche: Research Funding; TG therapeutics: Research Funding; BeiGene: Research Funding. Arnason:Regeneron Pharmaceuticals, Inc.: Consultancy; Celgene/Juno: Consultancy. Brown:Sun Pharmaceuticals: Research Funding; Janssen: Honoraria; Teva: Honoraria; Morphosys: Other: Data safety monitoring board; Invectys: Other: Data safety monitoring board; Octapharma: Consultancy; Pharmacyclics: Consultancy; Sunesis: Consultancy; TG Therapeutics: Consultancy; Verastem: Consultancy, Research Funding; AbbVie: Consultancy; Acerta Pharma: Consultancy; AstraZeneca: Consultancy; BeiGene: Consultancy; Catapult Therapeutics: Consultancy; Dynamo Therapeutics: Consultancy; Genentech/Roche: Consultancy; Gilead: Consultancy, Research Funding; Juno/Celgene: Consultancy; Kite, a Gilead Company: Consultancy, Research Funding; Loxo: Consultancy, Research Funding; Novartis: Consultancy; Pfizer: Consultancy. Davids:Research to Practice: Honoraria; AbbVie, Acerta Pharma, Adaptive, Biotechnologies, Astra-Zeneca, Genentech, Gilead Sciences, Janssen, Pharmacyclics, TG therapeutics: Membership on an entity's Board of Directors or advisory committees; AbbVie, Astra-Zeneca, Genentech, Janssen, MEI, Pharmacyclics, Syros Pharmaceuticals, Verastem: Consultancy; Acerta Pharma, Ascentage Pharma, Genentech, MEI pharma, Pharmacyclics, Surface Oncology, TG Therapeutics, Verastem: Research Funding.
Duvelisib and venetoclax are approved for the treatment of CLL, but not in combination
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal