Introduction: Tyrosine kinase inhibitor (TKI) therapy can result in the adverse events of prolonged anemia, thrombocytopenia and/or leukopenia via c-kit blockade in hematopoietic stem cells. Previous studies have reported that even low-grade adverse events could impair a patient's health-related quality of life. One of the benefits of TKI discontinuation is to allow patients to live drug-free, thereby preventing drug-related adverse events including cytopenias. The Canadian tyrosine kinase inhibitor (TKI) discontinuation trial has reported 59.1% and 21.5% molecular relapse-free survival (mRFS) rates after first and second attempts at treatment free remission (TFR) with imatinib (IM) or Dasatinib (DA) discontinuation, respectively. In the present study, we attempted to analyze the impact of TKI discontinuation on changes in hematological parameters, and its impact on TFR success after TKI discontinuation.
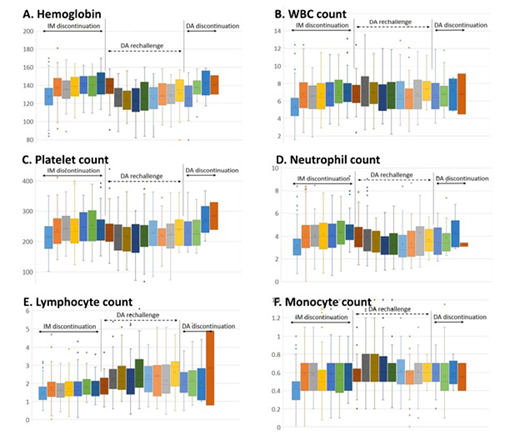
Methods and materials: Throughout the trial, we have collected the hematoloigc parameters at 22 timepoints in 131 patients. These included Hb level, WBC count with differentials, and platelet count during IM discontinuation (7 times), DA rechallenge (10 times), and DA discontinuation (5 times).
Results: With IM discontinuation, most of the hematological parameters showed a significant improvement within 3 months: Hb level rise by +10.47g/L (+8.86%; p=1.67x10-22), WBC count rise by +1.43x109/L (+30.08%; p=2.03x10-16), neutrophil rise by +0.99x109/L (36.76%; p=4.48x10-11), lymphocyte rise by +0.24x109/L (+20.64%; p=6.72x10-9), monocyte rise by +0.13x109/L (+35.9 0%; p=3.33x10-14), platelet count rise by +22.65 x109/L (+12.76%; p=1.03x10-7). Eosinophil counts were not significantly changed (p=0.475).
With DA rechallenge, mixed changes were observed in hematologic parameters within 1 month: Hb level significant dropped by 11.57g/L (-8.26%; p=6.38x10-14) and platelet counts also showed a decreasing trend (-9.39x109/L or -4.57%; p=0.07), while significant increases were noted in lymphocyte (+0.41x109/L or +22.22%; p=0.00027), and monocyte counts (+0.14x109/L or +14.29%; p=0.001). No significant changes were noted in WBC counts (+0.32x109/L or +1.64%; p=0.234), neutrophil counts (-0.18x109/L or -10.42%; p=0.285), or eosinophil counts (+0.03 x109/L or 0%; p=0.185).
With DA discontinuation, the Hb level rebounded by +7.08g/L within 3 months (+9.45%; p=0.0003). However, there was no significant change in the other parameters 3 months after DA discontinuation, including WBC (p=0.841), neutrophil (p=0.309), lymphocyte (p=0.995), monocyte (p=0.451), eosinophil (p=0.826) and platelet counts (p=0.533).
When the changes in hematologic parameters were analyzed in correlation with mRFS, there was no association of those parameter changes with RFS after DA discontinuation. However, associations of mRFS following IM discontinuation were noted as follows: higher mRFS after IM discontinuation was observed in the group with a smaller change in Hb level (≤+1.17%, p=0.004), lymphocyte count (≤+1.06%; p=0.006), and monocyte count (≤+1.43%; 0.005) compared to those with a larger change. In other words, the group showing a rebounded Hb level after IM discontinuation showed a lower mRFS rate compared to those in whom the Hb did not rebound. A lower mRFS was noted in the group with a smaller change in neutrophil count (≤+1.07%) compared to those with a larger change (p=0.008), implying that the group with rebounded neutrophil count showed a higher mRFS compared to those not.
Multivariate analysis confirmed: 1) IM treatment duration longer than 8.75 years is associated with a decrease in loss of molecular response by 13% per year (p=0.001, HR 0.871), 2) Hb level rebound above 22gm/L showed 2.8 times higher risk of molecular relapse (p=0.021, HR 2.801), 3) rebound rise of neutrophil count by 1.075% or above reduced the risk of molecular relapse by 52% (p=0.06, HR 0.485).
Conclusion: Further research is warranted to explore the functional role of the hematopoietic stem cell fraction following prolonged TKI therapy in CML patients. Hematopoiesis in Ph-negative cell population could contribute to TFR after TKI discontinuation.
Busque:ExCellThera: Patents & Royalties; BMS: Consultancy; Novartis: Consultancy; Pfizer: Consultancy; Paladin: Consultancy. Savoie:BMS: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Pfizer: Consultancy. Keating:Celgene: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria; Seattle Genetics: Consultancy; Janssen: Membership on an entity's Board of Directors or advisory committees; Shire: Membership on an entity's Board of Directors or advisory committees; Hoffman La Roche: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees. Delage:Celgene: Honoraria, Research Funding; Novartis: Honoraria, Research Funding. Liew:Novartis: Consultancy, Honoraria. Leber:Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees; Alexion: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal