Background: While there is evidence in the literature of increased prevalence of hypogammaglobulinemia in chronic lymphocytic leukemia (CLL), there are no studies evaluating the prevalence of hypogammaglobulinemia in newly diagnosed diffuse large B cell lymphoma (DLBCL) or the relationship between hypogammaglobulinemia and presentation or outcomes. The objective of this study was to examine the prevalence of hypogammaglobulinemia in newly diagnosed DLBCL patients and to test the hypothesis that DLBCL patients with baseline hypogammaglobulinemia have a distinct clinical profile and outcome.
Methods: We obtained banked frozen sera from 200 newly diagnosed, treatment-naïve, DLBCL patients from the Lymphoma SPORE Molecular Epidemiology Resource (MER), a prospective cohort study conducted at the Mayo Clinic and the University of Iowa. IgG/A/M levels were measured using immunoturbidimetric assay whereas IgE level was measured using electrochemiluminescence immunoassay; deficiency was defined using standard reference ranges. IgE levels were considered deficient if <2 UI/ml. The associations between Ig deficiencies and clinical factors were evaluated with Wilcoxon rank sum and chi-squared (Fisher's exact, where appropriate) tests. Event-free survival (EFS) was defined as time from diagnosis to progression, relapse, retreatment, or death, and EFS24 was defined as EFS at 24 months after diagnosis (achieve or failure to achieve EFS24). The association of Ig levels with EFS24 was estimated using odds ratios (OR) and 95% confidence intervals (CI) from logistic regression, and with EFS, overall survival (OS), and lymphoma-specific survival (LSS) was estimated using Kaplan-Meier curves and hazard ratios (HR) and 95% CI from Cox regression.
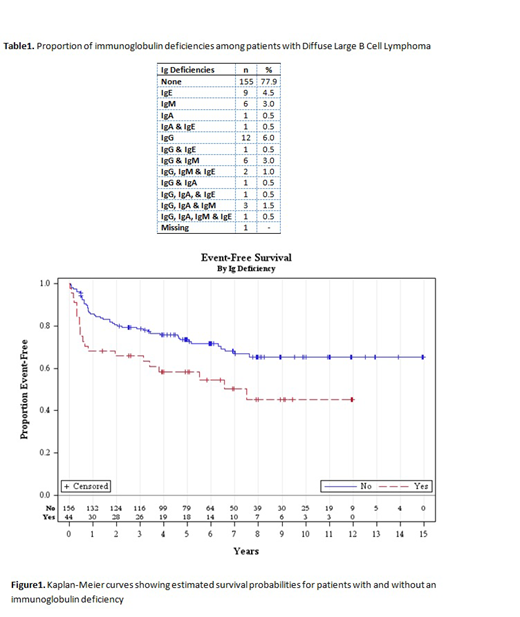
Results: The mean age (SD) of the cohort was 65.6 (13.4) years, 54% were males and 98% of the patients were white. Over a median follow-up of five years, there were 59 (29.5%) deaths. The prevalence of hypogammaglobulinemia, defined as any deficiency, in newly diagnosed, treatment-naïve DLBCL was 22.1% (44/199) in our cohort, and the most common Ig deficiency was for IgG (<700 mg/dL, 13.5%), followed by IgM (<40 mg/dL, 9.0%), IgE (<2 UI/ml, 7.5%) and IgA (<70 mg/dL, 4.0%) (Table1). There were no statistically significant differences between Ig deficient and non-deficient patients in terms of age at diagnosis, gender, stage, cell of origin, or MYC double hit status. However, median LDH levels were higher in Ig deficient patients (228 vs 194, p<0.01). Any immunoglobulin deficiency was associated with inferior EFS (HR 1.94, 95% CI 1.16-3.24) (Figure 1) and OS (HR 2.02, 95% CI 1.17-3.49), and these associations were not attenuated after adjustment for the international prognostic index (IPI). Any Ig deficiency was also associated with failure to achieve EFS24 (OR=2.13, 95% CI 1.00-4.60) after adjusting for IPI.
Conclusions: To the best of our knowledge, this is the first study to report the prevalence of hypogammaglobulinemia in treatment naïve DLBCL. We found that any Ig deficiency was not uncommon in our cohort and it was associated with an inferior EFS and OS in DLBCL patients. The prevalence of hypogammaglobulinemia in DLBCL patients seems to be lower than has been described in CLL patients. While the underlying relationship between these two immunologic disorders deserves further study, our findings highlight the interaction between global immune dysfunction and emergence of a clonal B cell process.
Nowakowski:Genentech, Inc.: Research Funding; F. Hoffmann-La Roche Ltd: Research Funding; Curis: Research Funding; Bayer: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Selvita: Membership on an entity's Board of Directors or advisory committees; NanoString: Research Funding; MorphoSys: Consultancy, Research Funding. Farooq:Celgene: Honoraria; Kite Pharma: Research Funding. Cerhan:NanoString: Research Funding; Celgene: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal