Introduction: The prognostic value of interim FDG-PET/CT (iPET) in classic Hodgkin lymphoma (cHL) was demonstrated in several clinical trials. Although in last decade the PET/CT has been cHL gold standard for the staging at diagnosis and final response evaluation, the introduction of an early interim evaluation in the management algorithms and guidelines is very recent. Therefore, there are few results concerning iPET prognosis significance in real-life setting.
We aimed to evaluate iPET predictor value in real-life cHL patients.
Methods: A single center retrospective study was performed on cHL patients diagnosed in 2005 to 2017, who underwent iPET after two cycles of quimiotherapy. Negative iPET (iPET-) was defined as a Deauville score≤3 (Lugano classification). We did not perform any adjustment in the treatment based on iPET, except when a disease progression was evident.
A p-value<0.05 was considered significant. The survival curves were compared using the log-rank test. The hazard ratios (HR) were estimated using univariate Cox proportional hazards regression models. All risk factors with p<0.15 in univariate model were further moved in multivariate analysis.
Results: We analyzed 463 patients, from whom 164 (36%) underwent an iPET; 56% were male and the median age was 34 years old (18-81).
The first line therapy, stratified according German Hodgkin Study Group (GHSG) group, was ABVD (n=124) [15% limited (LiS), 46% intermediate (InS) and 39% advanced stage (AdS)] and escalated BEACOPP (n=40) (20% InS and 80% AdS).
Considering response in iPET, 73% (n=120) presented an iPET- and 27% (n=44) a positive iPET (iPET+). No patient present evidence of disease progression. iPET+ proportion was similar between GHSG stages (24 vs 17 vs 32% respectively; p=NS). All other disease variables (Ann Arbor stage, International Prognostic Score [IPS], B-symptoms, bulky disease, bone marrow and extranodal infiltration and age) as well as treatment (iPET+ 27% ABVD vs 28% escalated BEACOPP; p=NS) did not reveal any significant difference between iPET- and iPET+.
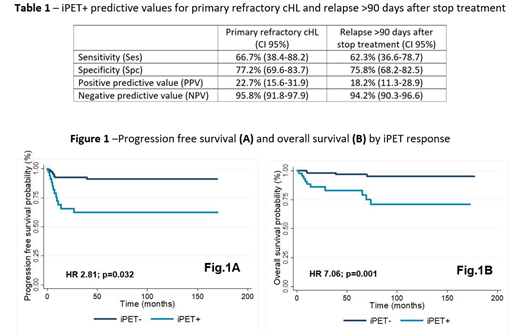
The overall response rate (ORR) was 91%. The iPET sensitivity for predicting primary refractory cHL (PR) and relapse >90 days after stop treatment (LateR) was 66.7% and 62.3%, respectively, for a negative predictive value (NPV) of 95.8% and 94.2%. The OR of iPET+ for predicting PR and LateR was 3.62 (95%CI 1.59-8.27) and 3.59 (95%CI 1.22-10.58), respectively (Table 1).
The progression free survival (PFS) at 10 years was 62% and 90% for iPET+ and iPET-, respectively, and PFS was significantly higher in iPET- group (HR 2.81; p=0.032), even in a sub-analysis of AdS patients, after stratifying for IPS (HR 1.81; p=0.006) (Figure 1A).
The overall survival (OS) for iPET+ and iPET- at 10 years was 71% and 95%, respectively, and OS was significantly higher in iPET- group (HR 7.06; p=0.001), even in the previous sub-analysis of AdS patients stratified by IPS (HR 2.93; p<0.001) (Figure 1B).
The negative impact of iPET positivity in PFS and OS remained significant, even after a multivariate analysis for different prognostic variables, namely age, Ann Arbor stage, GHSG stage and IPS (Ads only) (p=0.037 and p<0.001, respectively).
Conclusions: Our results validated the accuracy of iPET as an independent predictor for PFS and OS, even after adjusting for prognostic scores as IPS. In our cohort, iPET showed a higher specificity and negative predictive value, but a lower sensitivity and positive predictive value. These findings support the recent inclusion of iPET-guided strategies in the therapeutic algorithms.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal