Introduction
In MCL, progression-free survival (PFS) generally declines with each successive line of chemoimmunotherapy (CIT). We have previously published that with ibrutinib, a first-in-class oral inhibitor of Bruton's tyrosine kinase and a standard of care treatment (tx) for R/R MCL, median PFS exceeded 2 years (yrs) when used at first relapse (Rule S, et al. Haematologica. 2018;104:e211-e214). Here we present an updated pooled analysis with 15 months (mos) of additional follow-up, and for the first time, a comparison of outcomes with ibrutinib versus the prior regimen.
Methods
Patients (pts) enrolled in SPARK (MCL2001; NCT01599949), RAY (MCL3001; NCT01646021), and PCYC-1104 (NCT01236391) received ibrutinib 560 mg orally once daily until progressive disease or unacceptable toxicity, and pts benefiting at end of study could enroll in the open-label long-term extension study CAN3001 (NCT01804686). Tumor response (by Cheson B, et al; 2007 criteria) and PFS were investigator assessed. Positron emission tomography scans were not routine but confirmatory for complete responses (CRs). Disease evaluations in CAN3001 were per routine clinical practice and pts could continue tx as long as clinically benefiting. For the regimen prior to ibrutinib, time to next tx (TTNT: date of first dose of prior regimen to date of first dose of ibrutinib) was used as a surrogate for PFS. Progression of disease (POD) on frontline tx was categorized as early (TTNT < 24 mos) or late (TTNT ≥ 24 mos). Medians are reported with 95% confidence intervals (CIs).
Results
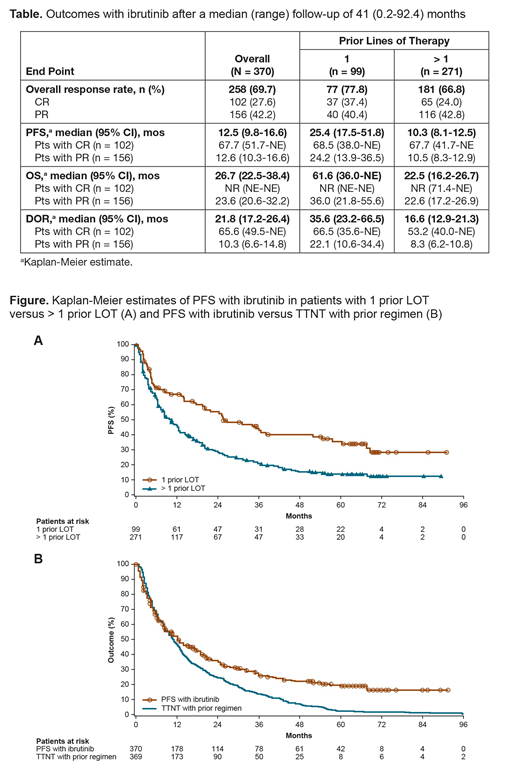
As of April 2019, the median (range) follow-up and exposure for 370 ibrutinib-treated pts (median 2 [range 1-9] prior lines of therapy [LOT]) were 41 (0.2-92.4) mos and 11.1 (0.03-92.4) mos, respectively, and 32/87 (37%) pts in CAN3001 remain on ibrutinib. Tx duration was ≥ 3 yrs in 22.4% of pts.
At 5 yrs, PFS and overall survival (OS) rates (95% CI) were 19% (15-24) and 41% (35-47), respectively. Pts with 1 prior LOT and pts achieving CR had the best outcomes (Table). Median PFS and OS in pts with 1 prior LOT were 25.4 (17.5-51.8) and 61.6 (36.0-not estimable [NE]) mos, respectively (Figure A). Median PFS and OS in pts with CR were 67.7 (51.7-NE) mos and NR (NE-NE) mos, respectively.
Overall, median PFS on ibrutinib was 12.5 (9.8-16.6) mos, while median TTNT on the prior regimen was 10.9 (9.1-12.6) mos (Figure B). PFS with ibrutinib was longer than TTNT on the prior regimen for 50% of pts and was ≥ 12 mos longer than TTNT on the prior regimen for 27% of pts. Factors ≥ 10% more common in pts achieving ≥ 12-mo longer PFS versus those who did not included low-risk simplified MCL International Prognostic Index (sMIPI), no extranodal disease, no bulky disease (≥ 5 cm), nonblastoid histology, TP53 wild type, and best response of CR.
Ninety-nine pts received ibrutinib in second line (44% ≥ 70 yrs old, 26% with high-risk sMIPI, 1% with Eastern Cooperative Oncology Group performance status ≥ 2, 6% with blastoid variant). Forty-three of 99 pts (43%) had early frontline POD and 56 (57%) had late frontline POD. In pts with early frontline POD, median PFS with ibrutinib (13.8 [4.3-24.2] mos) was similar to median frontline TTNT (14.0 [12.0-16.1] mos); median duration of response (DOR) and OS on ibrutinib were 22.1 (10.6-35.6) and 23.5 (10.3-61.6) mos, respectively. In pts with late frontline POD, median PFS with ibrutinib (57.5 [31.1-NE] mos) was longer than median frontline TTNT (42.2 [35.2-46.5] mos); median DOR and OS on ibrutinib were NE (33.1-NE) and NE (51.9-NE), respectively.
There was no late unexpected toxicity.
Conclusions
This pooled analysis of ibrutinib in R/R MCL with extended follow-up up to 7.5 yrs indicates a late plateau in the PFS curve with a significant number of pts experiencing remission > 5 yrs. Tx with ibrutinib in second versus later lines extended median PFS and increased likelihood of a CR. Pts achieving CRs with ibrutinib had durable responses, with a median duration > 5.5 yrs. Contrary to historical outcomes with CIT, half of all pts treated with ibrutinib experienced a longer PFS than with the prior regimen, and one quarter had ≥ 1 additional yr of benefit. In pts with early frontline POD, ibrutinib delivered a similar magnitude of PFS benefit in second line. In chemosensitive pts with late frontline POD, second-line ibrutinib PFS was 36% longer than frontline outcome. There was no notable emerging toxicity with additional follow-up.
Rule:Janssen: Consultancy, Honoraria, Research Funding; Roche: Consultancy, Honoraria, Research Funding; Astra-Zeneca: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Pharmacyclics: Consultancy, Honoraria; Gilead: Consultancy, Honoraria; Sunesis: Consultancy, Honoraria; TG Therapeutics: Consultancy, Honoraria; Napp: Consultancy; Kite: Consultancy. Dreyling:Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: scientific advisory board, Research Funding, Speakers Bureau; Janssen: Consultancy, Other: scientific advisory board, Research Funding, Speakers Bureau; Novartis: Other: scientific advisory board; Celgene: Consultancy, Other: scientific advisory board, Research Funding, Speakers Bureau; Bayer: Consultancy, Other: scientific advisory board, Speakers Bureau; Mundipharma: Consultancy, Research Funding; Acerta: Other: scientific advisory board; Gilead: Consultancy, Other: scientific advisory board, Speakers Bureau; Sandoz: Other: scientific advisory board. Goy:Pharmacyclics/Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Grants outside of the submitted work, Research Funding; COTA: Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Other: leadership role for profit healthcare company; Kite, a Gilead Company: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Grants outside of the submitted work; Takeda: Other: Grants outside of the submitted work; Genentech: Other: Grants outside of the submitted work, Research Funding; University of Nebraska: Research Funding; Hakensackumc: Research Funding; Astrazenca: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Hackensack University Medical Center, RCCA: Employment; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Acerta: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Grants outside of the submitted work, Research Funding. Hess:Celgene: Consultancy, Employment, Honoraria, Other: personal fees, Research Funding; Roche: Consultancy, Employment, Honoraria, Other: personal fees, Research Funding; CTI: Consultancy, Employment, Honoraria, Research Funding; Pfizer: Other: personal fees, Research Funding; Janssen: Consultancy, Honoraria, Other: personal fees; Novartis: Consultancy, Honoraria; MorphoSys: Consultancy, Honoraria. Auer:Hartley Taylor: Honoraria; Celgene: Other: personal fees; Janssen: Honoraria, Other: personal fees, Research Funding; Bristol-Myers Squibb: Other: personal fees. Kahl:Seattle Genetics: Consultancy; BeiGene: Consultancy; TG Therapeutics: Consultancy; ADC Therapeutics: Consultancy, Research Funding. Qi:Janssen: Employment. Deshpande:Janssen: Employment. Parisi:Janssen: Employment. Wang:Juno Therapeutics: Research Funding; VelosBio: Research Funding; Celgene: Honoraria, Research Funding; Aviara: Research Funding; Loxo Oncology: Research Funding; Dava Oncology: Honoraria; Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau; Pharmacyclics: Honoraria, Research Funding; AstraZeneca: Consultancy, Honoraria, Research Funding, Speakers Bureau; MoreHealth: Consultancy, Equity Ownership; Acerta Pharma: Consultancy, Research Funding; Kite Pharma: Consultancy, Research Funding; Guidepoint Global: Consultancy; BioInvent: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal