
Background
The Revised- International Prognostic Index (R-IPI), the current standard prognostic tool for patients with diffuse large cell lymphoma (DLBCL), considers only patient and clinical disease characteristics. The role of host immune homeostasis as an independent prognostic indicator in different diseases including DLBCL is evolving. Rambaldi et al 2013, showed that the lymphocyte monocyte ratio (LMR) at diagnosis is a simple prognostic biomarker and independent of the R-IPI. Low level of immunoglobulin at diagnosis, in particular IgG, is associated with inferior survival in Hodgkin and Non Hodgkin lymphoma patients (NHL). In DLBCL patients who underwent autologous transplants, Brown et al 2004 documented 18 months relapse free survival of 44% if IgG levels at time of transplant are below 600 mg/dL and 63% if higher. To our knowledge, the prognostic impact of immunoglobulin levels at diagnosis in patients with aggressive B-NHL has not been investigated. Therefore, we aimed to evaluate the prognostic role of the immunologic profile in terms of the pretreatment levels LMR and of immunoglobulins in patients with aggressive B-NHL.
Methods and results:
We retrospectively patients diagnosed with aggressive B non-Hodgkin lymphoma (NHL) at both the European Institute of Oncology in Milan and the Mauriziano Hospital in Turin from April 2014 to October 2018. Patients with DLBCL, Burkitt, Mantle cell and follicular G3B lymphomas were eligible. All patients were treated with chemo-immunotherapy according to center guidelines and a written informed consent was obtained from all them.
A total of 105 patients were included, with male predominance (60%), median age of 64.5 years (range 20-83) and ECOG score 0-1 in 66%. Stage III-IV disease was seen in 58%, extranodal involvement in 73%, bone marrow infiltration in 26%, bulky disease in 39% and high LDH in 66%.
Median IgG level was 1003 (range 436-2236) and the median LMR was 2.4 (range 0.2-44.2). By univariate analysis older age, advanced stage, higher ECOG PS, 2 or more extranodal disease sites, poor R-IPI, higher LDH, low LMR ratio as well as low IgG level at diagnosis was associated with a worse 1-year PFS. LMR inferior or equal to 2.4 had 1-year PFS of 70%, compared to 90% if LMR was higher (p 0.025). Patients with IgG levels less than 1003 had 1-year PFS of 70% compared to 90% in higher IgG levels. The later, didn' t reach statistical significance, due to small number of patients, but remains clinically relevant. Interestingly, there was no correlation between the levels of IgG and the LMR. Therefore, we examined the impact of combining each to R-IPI groups. A low IgG at diagnosis worsen the PFS in patients with good or very good R-IPI with 1 year PFS 83% (95% CI 60-93%) compared 97% (95% CI 79%-100%) if IgG levels are higher. Interestingly, patients in the poor IPI risk group and high IgG levels ad 1-year PFS similar to the good risk group with low IgG levels (PFS 84%, 95% CI 57-94%). The worst PFS is seen in the group of patients with poor IPI score and low IgG, PFS 61%, (95% CI 40%-77%). Similar results were seen in case of LMR.
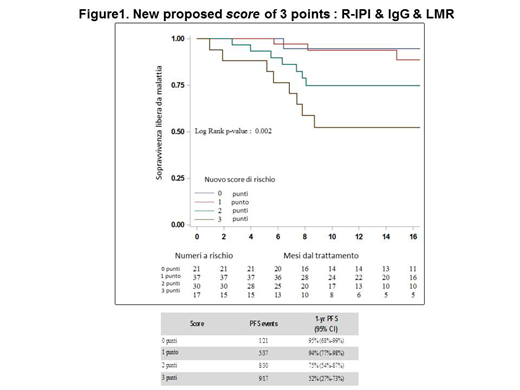
We then examined a novel immunologic prognostic score system that includes the three factors: baselines IGg levels, LMR and the R-IPI Figure 1. Because IgG levels and LMR are independent we put the same weight on each factor as well as the R-IPI score. We gave 1 point to each factor R-IPI poor (1 point) + IgG low (1 point) + LMR low (1 point). The sum of the chosen points correlated with four risk groups: group 1 = 0 points, group =2 = 1 point, group 3= 2 points and group 4= 3 points. The 1 year PFS was 95% (95% CI 68%-99%), 94% (95% CI 77%-98%), 75% (95% CI 54%-87%), 52% (95% CI 27%-73%), respectively.
Conclusion:
To our knowledge, this study is the first to report the prognostic implications of pretreatment levels of immunoglobulin IgG within the immunologic profile of patients with aggressive B-NHL. Our results suggests that IgG level at diagnosis is a clinically important prognostic factor. With the proposed immunologic score, patients are reclassified into four sub-groups with 3 significantly different 1-year PFS of 95% 75%, 50% in patients with no or one poor risk factor, 2 factors or 3 factors, respectively. This study confirms that the addition of baseline immunologic profile to R-IPI in patients with aggressive B-NHL optimizes their prognostic stratification and better identify patients who are at risk of poor outcome compared to the R-IPI alone.
Saglio:BMS: Consultancy; Novartis: Consultancy; Ariad: Consultancy; Incyte: Consultancy; Pfizer: Consultancy; Jansen: Consultancy; Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal