Introduction: Cytogenetic and molecular landscape at diagnosis and the depth of response to induction therapy are the most powerful prognostic tools available in patients with Acute Myeloid Leukemia (AML). Among the tests to measure Minimal Residual Disease (MRD), one of the most commonly used is flow cytometry. Nowadays, there is no consensus about optimal time for measurement and the threshold above which has greater prognostic value in AML, as well as its involvement in therapeutic management.
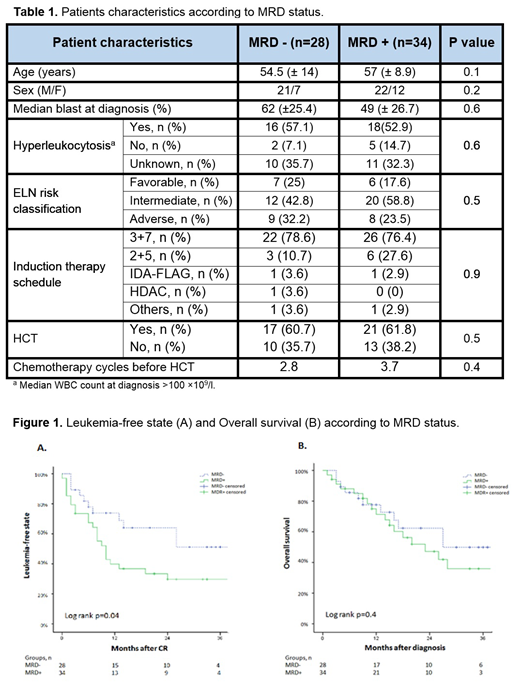
Material and methods: We performed a single-center retrospective analysis of 62 patients diagnosed with AML between 2015 and 2019 that reached complete remission after first induction. Patients were stratified according to the European Leukemia Net (ELN) risk classification. MRD measurement was made in bone marrow samples with an 8-color flow cytometer (sensitivity 10-5), cut-off 0.1%. We divided our cohort in two groups according to MRD after induction: negative MRD (MRD-) and positive MRD (MRD+). The baseline characteristics of each group were compared using the Chi2 test. The survival analysis was performed through Kaplan-Meier method and the risk was calculated with Cox regression. The Overall Survival (OS) was defined as the period of time from diagnosis to death and the leukemia-free state (LFS) as the period of time from CR to either relapse or death. Statistical analysis were carried out using SPSS version 19.0. P<0.05 was defined as statistically significant difference.
Results: Baseline characteristics of the sample are represented in Table 1. The median follow-up was 15 months (1-45). The 3-year LFS for MRD- and MRD+ was 50% and 29% respectively (figure 1A) showing a hazard ratio (HR) of 2.02 (CI 95% 0.98-4.6, p=0.05). The 3-year OS was 50% and 36% for MRD- and MRD+ respectively (figure 1B) and HR was 1.3 (CI 95% 0.6-2.8, p=0.4). In MRD+ group according to ELN risk classification, the 3-year LFS was 100% vs 21% vs 19% for favorable, intermediate and adverse risk, respectively (p=0.01) with a HR of 2.1 (CI 95% 1.1-3.9, p=0.01) in the univariate analysis. The 3-year OS was 100% vs 24% vs 18% for each subgroup (p=0.03) with a HR of 2.1 (CI 95% 1.06-4.4, p= 0.03). Thirty-eight patients received consolidation with hematopoietic stem cell transplantation (HSCT), and MRD prior to HSCT was measured in 32 of 38, being positive in 10 patients. All cases with MRD+ before HSCT belonged to MRD+ after induction group (10/20) (p=0.03). In MRD+ group, the 3-year LFS was 36% among those who received HSCT vs 18% in those who did not (log rank p=0.02, HR 3.1 CI 95% 1.3-7.8 p=0.01).
Conclusions: The persistence of MRD > 0.1% after first induction by flow cytometry has shown in our population the identification of a AML subgroup of high risk, specially relevant in the intermediate risk group of ELN classification. MRD+ leads to higher risk of relapse, and these patients benefit from more aggressive therapeutic strategies, including allogeneic HSCT. However, MRD+ group has more risk of MRD persistence prior to HSCT, the last being a knowing factor of relapse after allogeneic HSCT, what would justify more aggressive strategies after HSCT in these patients.
Piris-Villaespesa:Novartis: Honoraria, Other: Advisory Boards. García Gutiérrez:BMS: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; Incyte: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal