Background
Next-generation sequencing (NGS) panels have created an unprecedented opportunity to interrogate a broad array of variants in a multiplex fashion. Few data have demonstrated how NGS testing impacts diagnosis and treatment decisions. In this retrospective analysis, we evaluated the clinical application of NGS myeloid panels (MP) in patients (pts) evaluated by physicians in the Stanford Division of Hematology.
Methods
The study was approved by the Stanford University IRB. The cohort consisted of 1,015 pts ≥18 years of age (median 66; range 18-96 years; 51% female). A total of 1,213 MPs obtained from peripheral blood (n=568) or bone marrow (n=645) from March 2017 to June 2018 were analyzed at Stanford (n=761) using the 54-gene TruSight® Myeloid Sequencing Panel (Illumina, San Diego, CA) or Oregon Health & Science University (n=452) using the GeneTrails® Hematologic Malignancies 76-Gene Panel. Electronic medical records were reviewed from t-3 to t+9 months from when MPs were obtained to assess physician reasoning for MP acquisition, documentation of results, and how results were clinically applied. We defined three categories of MP acquisition: 1) diagnostic clarification, 2) prognostication and/or management guidance, or 3) minimal residual disease (MRD) monitoring. We analyzed changes in clinical management, including addition of targeted or non-targeted therapeutics, clinical trial eligibility, or other practice recommendations.
Results
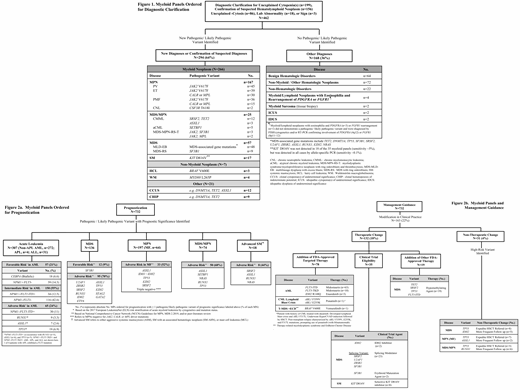
Of the 1,213 MPs, 882 (73%) demonstrated at least one pathogenic/ likely pathogenic variant (median 2; range 1-8). Median turn-around-time was 18 days (range 7-31) and average cost was $2,600. Of all MPs, 462 (38%) were obtained for diagnostic clarification, 732 (60%) for prognostication / management guidance in pts with known myeloid (n=701) or lymphoid (n=31) neoplasms, and 19 (2%) for MRD monitoring, although the assay was not designed for this indication. MPs were ordered to clarify a diagnosis for the following reasons: unexplained cytopenia(s) (n=199), molecular profiling for a suspected hematolymphoid neoplasm (n=156), unexplained -cytosis (n=86), and testing for other lab abnormalities (e.g. elevated serum tryptase, paraproteinemia) (n=18), or signs (e.g. splenomegaly, splenic vein thrombosis)(n=3). A pathogenic/likely pathogenic variant was found in 294 (64%) pts, confirming or establishing the presence of a myeloid (n=266) or lymphoid neoplasm (n=7) or resulting in a diagnosis of CHIP (n=9) or CCUS (n=12) in pts who did not meet 2016 World Health Organization diagnostic criteria for a hematolymphoid neoplasm (Fig. 1).
Of the 732 MPs ordered for prognostication/ management guidance, 272 MPs (37%) were obtained in the initial workup of non-APL AML pts. The frequency of favorable (21%), intermediate (55%), and adverse risk (24%) genetics according to the European LeukemiaNet stratification in non-APL AML is shown in Figure 2a, which also denotes the frequency of favorable (9%) or adverse risk (70%) variants in MDS, and adverse risk variants in MF (52%), MDS/MPN (68%), and advanced systemic mastocytosis (44%). Among MPs obtained for prognostication/ management guidance, 163 (22%) led to a modification in clinical practice, divided between 132 (18%) which led the physician to change therapy (e.g. FDA-approved targeted therapy, clinical trial, or FDA-approved therapy, such as hypomethylating agents in MDS) and 31 (4%) resulted in a non-therapeutic change (e.g. expedited HSCT referral or more frequent follow-up)(Fig. 2b).
87 pts with a myeloid neoplasm had 184 repeat MPs for relapsed/refractory disease (n=52), transformation to higher-risk MDS or AML (n=45) or progressive cytopenias (n=87). Among these MPs, 38 (21%) identified a new pathogenic/likely pathogenic variant of which 29% (n=11) led to either a) initiation of targeted therapy with enasidenib in relapsed IDH2+ AML (n=3) or midostaurin for secondary FLT3+ AML from MDS (n=3), or b) consideration for a clinical trial with a splicing modulator for MDS characterized by a splicing variant (n=5).
Conclusion
In our academic hematology practice, two-thirds of MPs ordered for diagnostic clarification identified a pathogenic/likely pathogenetic variant that helped to confirm or establish a new diagnosis of a hematolymphoid neoplasm, CHIP, or CCUS. In addition, approximately 20% of MPs ordered for prognostication/ management guidance led to a change in clinical practice.
Gotlib:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Blueprint Medicines: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Promedior: Research Funding; Pharmacyclics: Research Funding; Gilead: Membership on an entity's Board of Directors or advisory committees, Research Funding; Allakos: Honoraria, Membership on an entity's Board of Directors or advisory committees; Deceiphera: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Seattle Genetics: Research Funding; Incyte: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal