
Introduction: There is no consensus regarding the best salvage regimen for refractory or relapsed acute myeloid leukemia (r/rAML), with classic regimens traditionally based on high-dose cytarabine in a changeable combination with anthracyclines, purine analogs, and etoposide. Outcomes of r/rAML patients in developing countries are underreported, even though the same regimens are widely used.
Methods: This is a retrospective single-center study, conducted in an academic center in Brazil. Local research ethics committee approved this analysis. All patients above 16 years of age who received MEC (mitoxantrone, etoposide and cytarabine) or FLAG-IDA (fludarabine, cytarabine, filgrastim and idarubicin) as originally reported (Amadori, S. et al. and Steinmetz, H. T. et al.) for r/rAML between December/2009 and January/2019 were included. Only patients with refractory or relapsed disease following standard upfront therapy ("7+3" regimen) were included in this analysis, being divided among refractory (less than partial response after one cycle of "7+3"), early relapsed (relapse within one year from first complete response [CR]) and late relapsed (relapse after one year of CR). Only the first salvage was considered for this study.
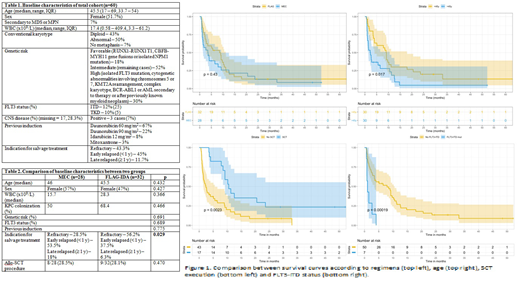
Results: Sixty patients were included in the final analysis, with a median age of 45 years (range, 17 - 69). There were no cases of therapy-related AML. Four AML cases (7%) were secondary to myeloproliferative neoplasm (MPN) or myelodysplastic syndrome (MDS). All FLT3-ITD positive cases had an associated NPM1 mutation. Two patients had chronic human immunodeficiency virus infection and received antiretroviral therapy. Baseline characteristics of the whole cohort are summarized in Table 1. Three patients had undergone SCT in first CR and were post-SCT relapses. Twenty-eight patients received MEC and 32 received FLAG-IDA. By comparing the baseline characteristics of both groups, no difference statistically significant was found except for the indication for salvage treatment, in which there were more refractory cases in FLAG-IDA group (56 vs. 28%, p=0.029) (Table 2). Overall, 17/60 achieved CR and 12/60 CRi, with a total CR rate (CR+CRi) of 48.3% (95% confidence interval [CI], 35.4 - 61.5). Sixteen patients (27%) early died before a response assessment. By univariate analysis, only age affected the CR rate (p=0.045). No difference in CR rate was found between the two protocols (MEC 53.5 vs. FLAG-IDA 43.7%, p=0.447). Looking into this data, it can be seen that there were more refractory patients in FLAG-IDA arm (37.5 vs. 4%, p=0.02) but more patients early-died in MEC arm (35.7 vs. 18.7%, p=0.137), even though the latter was not statistically significant. After correcting the initial differences between the two groups regarding indication for salvage through a propensity score calculation, a post-matching cohort with 44 subjects was found. In this cohort, no difference in refractoriness rate could be detected (p=0.077). In the whole cohort, 17 patients proceeded to allogeneic SCT - 15 in CR/CRi and 2 with active disease, with no difference in SCT execution rate between the two groups (p=0.470). 4/17 transplanted patients were alive. Median follow-up was 48 months. Median survival for total cohort was 4 months (95% CI, 2.7 - 9.2), with a 3-year OS of 9.7% (95% CI, 4 - 23.7) and a 3-year EFS of 7.5% (95% CI, 2.5 - 22.4). In the univariate analysis for OS, age (p=0.04), FLT3 status (p<0.001) and SCT procedure (p=0.002) were statistically significant. Chosen regimen did not influence OS or EFS as well as the genetic risk, colonization or time of relapse (Figure 1). In a multivariable model for EFS including age, FLT3 status and SCT procedure, only the last two indicators remained significant: FLT3-ITD mutation (Hazard ratio [HR] = 4.6 [95% CI 1.9 - 11.4], p<0.001) and SCT procedure (HR = 0.43 [95% CI 0.22 - 0.82], p=0.01).
Conclusion: In this analysis, there was no difference concerning the chosen regimen for r/rAML, even though a possible higher refractoriness rate could be seen in FLAG-IDA arm. High early toxicity was found, emphasizing the role of supportive care and judicious selection of patients to intensive salvage therapy in our setting. FLT3-ITD mutation and SCT remained as significant factors for survival in a multivariable analysis, which is in line with previous studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal