
Introduction: Five-year survival following childhood acute myeloid leukemia (AML) has doubled over the last 4 decades due to advances in treatment and supportive care, including more widespread use of hematopoietic cell transplantation (HCT). The impact on long-term morbidity and mortality among survivors is unknown.
Methods: Cumulative incidence and 95% confidence intervals (CI) for overall and cause-specific late (>5 years from diagnosis) mortality and CTCAE grades 3-5 chronic health conditions (CHC) were estimated among 5-year survivors of AML diagnosed <21 years of age between1970-99 in the CCSS. Comparisons were made by decade of diagnosis (1970s, 1980s, 1990s) and treatment (HCT vs. chemotherapy only [chemo-only]). Cox regression models estimated hazard ratios (HR) for health-related deaths and CHC based on treatment decade and HCT status.
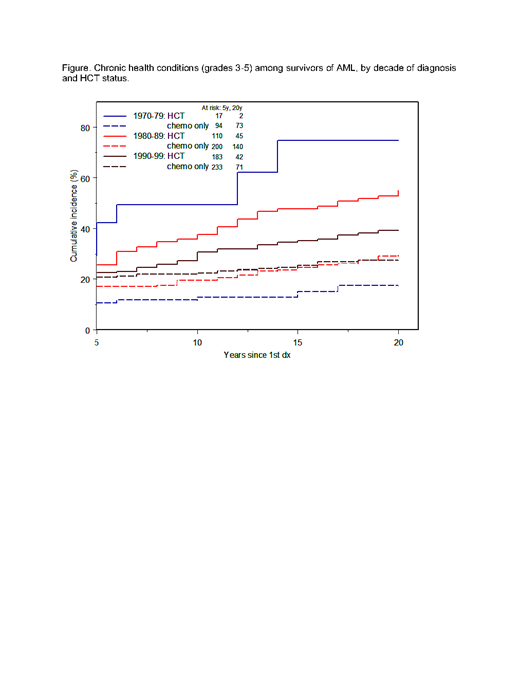
Results: Among 927 AML survivors (median age at diagnosis 7.1 years [range 1-21 years]; median age at last follow-up 29.4 years [range 8-60 years]; 16,069 person-years of follow-up; 37% treated with HCT [15% of 1970s survivors, 36% of 1980s survivors, 44% of 1990s survivors), the 20-year cumulative incidence of all-cause mortality was 6.7% (CI 4.2-9.2%) for chemo-only survivors and 13.5% (CI 9.2-17.8%) for HCT survivors. For chemo-only survivors, the highest incidence of health-related mortality were attributable to cardiac causes (1.5%, CI 0.5-2.6), relapse (0.9%, CI 0.1-1.8), and SMN (0.6%, CI 0.0-1.2), whereas for HCT survivors the highest health-related causes of death were relapse (6.5%, CI 3.7-9.2%), SMN (1.3%, CI 0-2.5%), and pulmonary causes (0.6%, CI 0-1.5%). When treatment groups were considered in multivariable Cox models, risk for late mortality was similar for chemo-only survivors from the 1990s compared to the 1970s (HR 0.4, CI 0.1-1.4), but risk was reduced for HCT survivors from the 1990s compared to the 1970s (HR 0.2, CI 0.1-0.4). The 20-year cumulative incidence of grade 3-5 CHCs among chemo-only survivors was 26.9% (CI 23.0-30.7%) compared to 46.8% (CI 40.9-52.7%) among HCT survivors, with the highest incidence occurring for cardiovascular CHC (chemo-only, 9.7%, CI 7.1-12.2%; HCT, 10.6%, CI 7.0-14.2%), pulmonary CHC (chemo-only, 1.0%, CI 0.1-1.9%; HCT, 2.9%, CI 1.0-4.8%) and SMN (chemo-only, 0.8%, CI 0.0-1.7%; HCT, 5.7%, CI 2.9-8.6%). Incidence of overall CHC decreased in more recent decades among HCT survivors (p=0.03, Figure); however, among chemo-only survivors, CHC incidence did not significantly change by decade (p=0.12). When treatment groups were considered in adjusted models, risk for CHC was similar for those treated in the 1990s compared to the 1970s among chemo-only survivors (HR 1.5, CI 1.0-2.3) and risk estimates among HCT survivors decreased over time but did not achieve statistical significance (HR 0.6, CI 0.3-1.1).
Conclusions: AML survivors treated with HCT had a reduced risk of late mortality and serious CHC in more recent treatment eras. In contrast, treatment with chemo-only was not associated with differences in mortality and serious CHC risk over time. Five-year survivors treated with chemo-only had a significantly reduced risk of health-related mortality compared with HCT survivors across all treatment eras. While treatment intensification with HCT has improved the cure rates for AML in recent decades, there remains disparity in long-term outcomes among AML survivors treated with HCT vs. chemo-only.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal