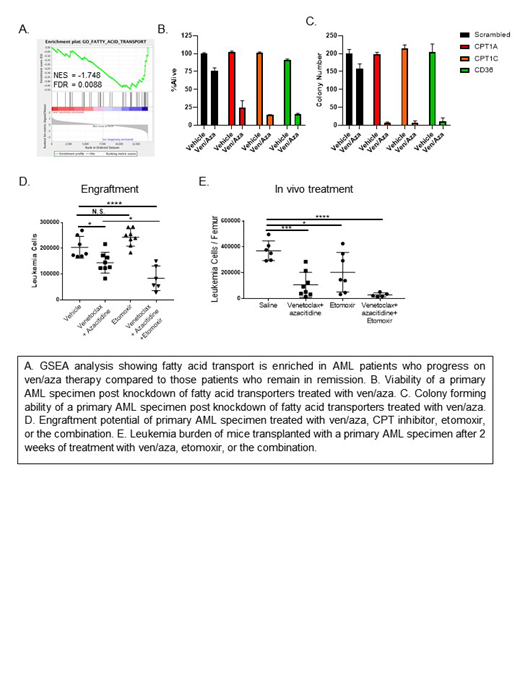
The combination of venetoclax with hypomethylating agents has resulted in highly promising clinical outcomes for acute myeloid leukemia (AML) patients. However, a subset of patients are refractory or develop resistance to venetoclax based regimens, resulting in disease recurrence. The goal of this project was to determine a mechanism to re-sensitize resistant leukemia stem cells (LSCs) to venetoclax with azacitidine (ven/aza) treatment. LSCs are the population of leukemia cells that initiate disease and are not fully eradicated by conventional treatments resulting in disease recurrence. We have previously reported that ven/aza targets LSCs in de novo AML patients by perturbing amino acid uptake resulting in decreased oxidative phosphorylation (OXPHOS). To investigate how some AML patients, develop resistance to ven/aza, we first determined if ven/aza reduced amino acid uptake in primary human AML ven/aza resistant LSCs by stable isotope labeled metabolic flux and mass spectroscopy analysis. Amino acid uptake was significantly reduced in both ven/aza sensitive and resistant LSCs upon ven/aza treatment, indicating that ven/aza is still biologically active in resistant LSCs. Next, we performed gene expression analysis from LSCs isolated from AML patients who were treated with ven/aza, responded, and then either remained in remission or progressed on ven/aza therapy. Gene set enrichment analysis revealed that fatty acid transport was enriched in LSCs isolated from patients who eventually progressed on ven/aza therapy (FDR = 0.0088) (Figure A). We then determined differences in overall fatty acid levels by lipidomics mass spectroscopy analysis in ven/aza sensitive and resistant LSCs. We observed a significant increase in abundance of 20% (6/29) of fatty acids detected in resistant LSCs. To determine if targeting fatty acid transport could re-sensitize resistant LSCs to ven/aza we knocked down genes involved in fatty acid transport including CD36, CPT1A and CPT1C in 4 ven/aza resistant AML specimens and then measured viability and colony-forming potential upon ven/aza treatment (Figure B and C). Knockdown of CD36, CPT1A, or CPT1C in combination with ven/aza treatment significantly decreased both viability and colony forming ability in each of the AML specimens. In addition, knockdown of CPT1A or CPT1C in combination with ven/aza reduced OXPHOS, a known metabolic requirement of LSCs.
To perturb fatty acid transport in a therapeutically relevant manner, we treated LSCs isolated from ven/aza resistant patient specimens with a CPT1 inhibitor, etomoxir, as a single agent or in combination with ven/aza, and then measured viability and OXPHOS. The combination but not single agents reduced viability and OXPHOS, consistent with our genetic studies. To determine if ven/aza with etomoxir targeted functional LSCs we treated a primary AML specimen with etomoxir, ven/aza or the combination and measured engraftment into immune deficient mice. Combination therapy significantly reduced engraftment potential compared to ven/aza or etomoxir alone indicating that the combination of ven/aza with etomoxir decreased LSC function (Figure D). To determine if ven/aza with etomoxir could target AML cells in vivo, we treated a primary patient derived xenograft model with ven/aza, etomoxir, or the combination for 2 weeks and measured leukemic burden in the bone marrow (Figure E). The combination reduced leukemic burden more significantly than ven/aza or etomoxir alone. Finally, we measured the consequences of ven/aza, etomoxir, or the combination on normal hematopoietic stem and progenitor cells. Neither single agents nor combination therapy decreased CD34+ cell viability or colony forming ability, indicating that there may be a therapeutic window to targeting these metabolic pathways in AML without harming normal stem cells. Gene expression analysis revealed that CD36, CPT1A, and CPT1C are expressed at significantly higher levels in AML compared to HSCs, which may contribute to this therapeutic window.
In conclusion, these data indicate that ven/aza resistance can be overcome by targeting fatty acid transport in LSCs. Furthermore, combining ven/aza with a CPT1 inhibitor such as etomoxir may be a clinically relevant strategy to overcoming ven/aza resistance.
Pollyea:Gilead: Consultancy, Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celyad: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Astellas: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Forty-Seven: Consultancy, Membership on an entity's Board of Directors or advisory committees; Diachii Sankyo: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal