Background: Prophylactic platelet transfusion is commonly used to prevent life-threatening bleeding events in patients with severe thrombocytopenia associated with chemotherapy courses or hematopoietic stem cells transplantation (HSCT). In adults, the transfusion threshold for prophylaxis is usually set at 10x109plts/L, but in pediatric setting, it is still a matter of debate. Moreover, evidences from the PLADO trial (Slichter SJ et al. N Engl J Med. 2010) and recommendations form international guidelines (ICTMG, Nahirniak S et al. Transfus Med Rev. 2015) suggest two different platelet doses in Inpatients and Outpatients, but clinical experiences in children are still lacking.
Aims: In order to confirm the safety of the recommended transfusion threshold, to test two different platelet doses in hospitalized patients and Outpatient setting and to optimize platelet clinical use, as a Children's Hospital, we applied, starting from January 2018, a new prophylactic platelet transfusion policy.
Methods: Platelet dose was calculated based on body-surface area (BSA) of each patient (from age-standardized weight). As suggested by ICTMG, different platelets doses were given to Inpatients and Outpatients: (low-dose) 1.1x1011platelets per square meter (plts/m2) and (medium-dose) 2.2x1011plts/m2, respectively. The transfusion threshold for prophylaxis was set at 10x109plts/L, but higher threshold could be considered as per clinical decision (in presence of bleeding signs or risk factors for major bleeding). Patients with platelets refractoriness and newborns, were excluded from our study. Only major bleeding events (grade 3 or higher according to World Health Organization criteria) were collected during the study period.
Results: From January 2018 to June 2019, 15278 platelet pediatric aliquots were transfused in our Hospital. Of all the aliquots, 8876 (58.1%) were obtained from apheresis procedures and 6402 (41.9%) from buffy-coat-derived pooled platelet concentrates. Almost 77% (11751) of the all aliquots were transfused in patients with onco-hematologic diseases.
Among these, 9771 (64.0%) in the Inpatient group (N=547) and 1980 (13.0%) in the Outpatient group (N=385). Between Inpatients, 6794 (44.5%) aliquots were transfused in Onco-Hematology Ward and 2977 (19.5%) in the HSCT unit.
During the study period, only 10 major bleeding events were observed. No fatal hemorrhagic episode was recorded and all of the bleedings occurred in hospitalized patients, and accounted for almost 2% of this population.
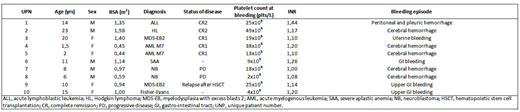
Intracranial bleeding accounted for five out of six grade 4 bleeding episodes, and occurred in two patients with acute myelogenous leukemia, in one patient with Hodgkin lymphoma and in two patients with advance neuroblastoma. The other grade 4 bleeding event was a massive peritoneal and pleuric hemorrhage with a life-threatening haemodinamic instability in a patient with acute lymphoblastic leukemia (the main characteristics of these patients are reported in the table).
Conclusions: our results show that a platelet transfusion policy based on recommendation mainly developed in adults may be safely applied also to pediatric patients with cancer or receiving HSCT. In fact, the lower dose used in Inpatient group resulted in a grade 4 bleeding rate similar to that observed in the PLADO trial (1.0% vs 0.7%). The double dose transfused in Oupatients was effective in preventing major bleeding events.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal