Introduction:
Gestational thrombocytopenia (GT) is one of the most common hematologic disorders of young adults, observed in approximately 10% of pregnancies worldwide. Despite its prevalence, the cause of GT is not known. To gain insight into the potential mechanisms underlying GT, we analyzed clinical and laboratory features of the 3,730 pregnancies delivered at the Massachusetts General Hospital in 2017.
Methods:
Patients were identified and their clinical data were extracted from a standardized obstetric database. Results of 25,131 complete blood counts (CBCs) were obtained directly from the hospital laboratory record. CBCs obtained prior to pregnancy were removed from analysis. GT was defined as women with at least one recorded platelet count of <150K at any time during day -100 to the day of the delivery (day 0). For CBCs obtained on day 0, the medical record was reviewed to ensure that only platelet counts prior to parturition were used to categorize the patient. Controls included all other patients with platelet counts >150K during the final 100 days antepartum. For both GT and controls, women with an ICD-9 code for pre-eclampsia, antiphospholipid antibody syndrome, ITP, SLE, HIV, HCV, or HBV were excluded (n=29), as were women with a platelet count <50K (n=6) at any time during the pregnancy. This method resulted in 3,695 deliveries available for analysis. Comparisons of GT versus controls used the chi-square test for categorical data, t-test for parametric data, and Wilcoxon test for non-parametric data.
Results:
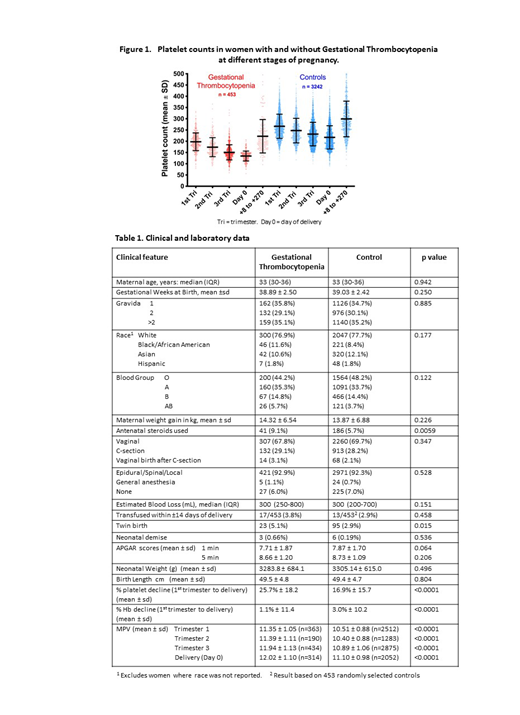
Of 3,695 deliveries, we identified 453 (12%) as GT and 3,242 as controls. For each stage of pregnancy, the CBC closest to delivery was selected, yielding 13,792 total CBCs for analysis (Figure 1). Of particular importance, the average percent decline in platelet count between trimester 1 and day 0 was 25.7% in women with GT versus 16.9% in the controls (p<0.0001). The decline in platelet count in both groups is much greater than the decline observed in hemoglobin (Hb) between trimester 1 and day 0: 1.1% decline in GT and 3.0% decline in controls. As shown in Table 1, the mean platelet volume (MPV) increased during pregnancy in both groups, with GT patients having a significantly higher MPV compared with controls in each trimester and at delivery (p<0.0001). Among 51 GT women with >1 CBC result post-partum, analysis revealed a greater than two-fold rise in platelet count within the first 7 days. The mean increases in platelet count compared with day 0 were: 100% on day 1, 117% on day 2, 142% on day 3, 159% on day 4, 187% on day 5, 214% on day 6, and 226% on day 7.
Clinical and demographic data for the 2 groups are shown in Table 1. There was no significant difference between GT and controls in maternal age, gestational weeks at delivery, gravida, race, blood type, weight gain, mode of delivery, type of anesthesia, estimated blood loss, transfusions, rates of neonatal demise, APGAR scores, neonatal height or weight. A higher percentage of GT patients (9.1%, n=41) were given antenatal steroids versus controls (5.7%, n=186) (p=0.0059). There were more twin pregnancies among the GT group (5.1%, n=23) versus controls (2.9%, n=95) (p=0.015).
Conclusions:
Based on this retrospective analysis of 3695 pregnancies, GT is confirmed as a common hematologic disorder, occurring in 12% of pregnancies in this series. The significantly greater percent-decline in platelets during pregnancy in women with GT compared with controls suggests that GT is a distinct pathophysiology, and not that all pregnancies result in a similar degree of platelet decline with GT women simply starting at a lower platelet count. The data also argue against hemodilution as the etiology for GT given the relative stability in Hb compared with platelet decline throughout gestation in both groups and given the lack of significant difference in maternal weight gain between GTs and controls. The rapid doubling in platelet count within 7 days of delivery argues against an autoimmune mechanism, which would not likely demonstrate such spontaneous recovery kinetics. The progressive and statistically significant increase in MPV in women with GT compared with controls would be consistent with a high platelet turnover state in affected women, which may be exaggerated in pregnancy by increased blood flow sheer rates. Exploring causes for an increased rate of platelet turnover in GT as a component of the responsible mechanism merits further investigation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal