Introduction
Sickle cell disease (SCD) is an autosomally, recessive inherited hemoglobinopathy and multisystem disorder characterized by ongoing hemolytic anemia, episodes of vaso-occlusion and progressive organ failure with ultimately a shortened life expectancy. Despite intensive comprehensive care and improved rates of morbidity and mortality, SCD care is still marked by high utilization of medical resources. Until now, most cost-of care studies have focused on one or two care categories, such as hospitalizations and physician visits [1-4]. Also, few studies have evaluated healthcare expenditures exclusively in children. Estimating cost-of care is important as it can ensure sufficient allocation of resources. In addition, SCD expenditures can be used to raise awareness of disease severity and serve as an incentive for prevention and management of disease complications. Primary aims of this study were to (a) investigate the overall cost of healthcare for pediatric SCD patients and to (b) estimate major cost drivers.
Methods
All pediatric SCD patients visiting the Erasmus University Medical Center-Sophia Children's Hospital for routine or emergency care from January 1st to December 31st 2017 with a diagnosis of SCD were included. Retrospective data of this cohort were analyzed for 24 months during January 1st 2015 to December 1st 2016. Patients were grouped into four age categories; (A) 0-12 months, (B) 1-5 years, (C) 5-13 years and (D) 13-19 years. For patients born before January 1st 2015, each individual contributed two years of follow-up time. As some children were born during one of the two years during the study time period, the weighted average was calculated based on the time patients were potentially able to make costs.
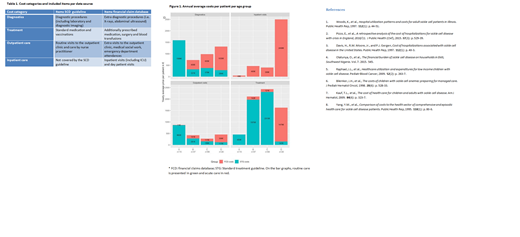
Healthcare utilization of included patients was based upon data from two main sources. The clinical SCD standard treatment guideline was used to determine the expected resource use of routine comprehensive care (planned elective care) and the Erasmus University Medical Center financial claims database was used to estimate real-world resource use associated with acute and inpatient care (additional care). The included items for the SCD guideline and financial claims database per cost category are summarized in Table 1.
Results
A total of 125 patients were analyzed. The mean age was 8.1 years (SD: 5 years) on December 31st 2015 and 9.9 year (SD: 5 years) on December 31st 2016. Expenditures for the 125 children with SCD averaged €4285.09 (SD: €820.36) per child per year. The majority (49%) of costs was associated with standard treatment (i.e. prophylactic antibiotics); 23% with diagnostics; 19% with inpatient hospital care and 9% with outpatients visits. Annual average costs per patient per age group are depicted in Figure 1. Total expenditures for children with SCD increased per age group, ranging from €2962 (category A), €3726 (category B), and €4087 (category C) to €5890 (category D). This was mostly explained by increases in admission costs.
Discussion
Although healthcare utilization and costs of pediatric SCD patients have been studied previously [5-7], studies from Europe comprehensive care centers are scarce and have been mostly based on only one aspect of care such as hospitalizations costs [2]. To our knowledge, this is the first study combining standard treatment costs with real world resource use. The total annual coast of healthcare for children with SCD, including inpatient care, outpatient care, diagnostics and treatment averaged €4285.09 per patient per year. This is much lower when compared to costs of healthcare for pediatric patients with SCD reported in other studies. Kauf et al. calculated total costs of healthcare for SCD patients aged 0-9 years to be $10.704 [7]. In addition, inpatient care accounts for a relatively small part of total costs in our study. This finding has been inline with previous research where comprehensive care has been suggested as a means of reducing costs associated with SCD care [8]. A comprehensive, multidisciplinary approach is necessary to address the physical, mental and social needs of each child and their family. Comprehensive care, with effective management in the outpatient setting is able to prevent hospital admission, and is essential for delivery of high quality cost-effective care in SCD.
Cnossen:Pfizer: Other: Travel Grants, Research Funding; Bayer: Other: Travel Grants, Research Funding; Novo Nordisk: Research Funding; Nordic Pharma: Research Funding; CSL Behring: Other: Travel Grants, Research Funding; Sobi: Research Funding; Baxter: Other: Travel Grants, Research Funding; Shire: Other: Travel Grants, Research Funding; Takeda: Other: Travel Grants, Research Funding; Roche: Other: Travel Grants; NWO: Other: Governmental grants , ZonMW, Innovation fund and Nationale Wetenschapsagenda 2018.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal