Children with sickle cell disease (SCD) have an increased risk of neurological complications, including stroke, silent cerebral infarction, and cognitive deficits. Past research by others has also shown increased risk for neurodevelopmental disorders (NDD) in this population (PMID 19142770, 27038278). A previous study conducted by our group noted that only 22% of patients with SCD and NDD had a prior history of stroke (PMID 26149844).
We investigated the prevalence and features of NDD in pediatric SCD through a retrospective chart review conducted between July 2017 and January 2019. The participants were patients with SCD identified from the Johns Hopkins Pediatric Hematology Harriet Lane Clinic roster and the Kennedy Krieger Institute medical records database. Children under 18 years of age with SCD were included in the study. A total of 396 patients were identified and reviewed for study inclusion. Analyses were completed using non-parametric tests (Wilcoxon-Mann-Whitney test, chi squared test) in Stata IC-13.
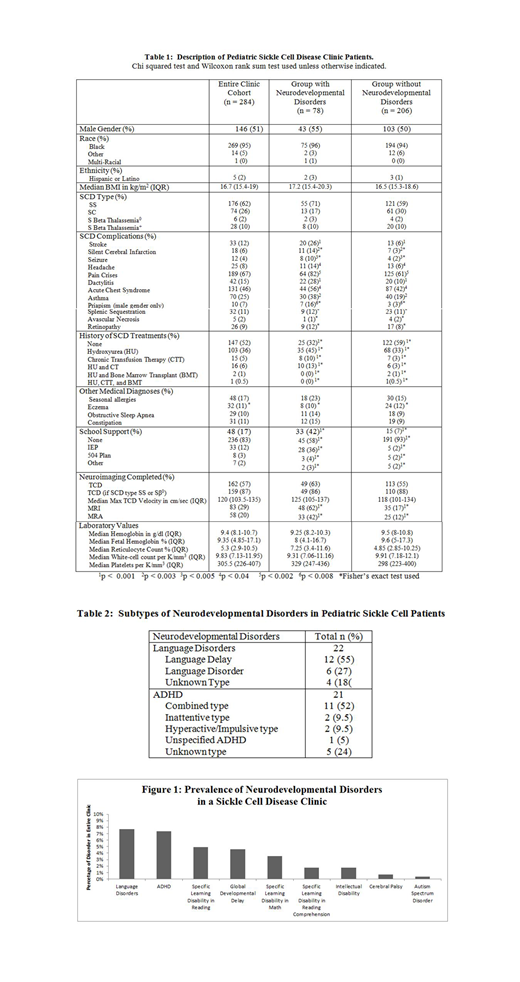
Table 1 shows the characteristics of the clinic patient population. A total of 284 participants qualified for study inclusion and 78 participants (27%) were found to have various NDD. Children with SCD and NDD were more likely to have a history of seizure (OR=5.77, 95%CI:1.69-19.76, p<0.006), stroke (OR=5.12, 95%CI:2.4-10.92, p<0.001), dactylitis (OR=3.65, 95%CI:1.86-7.18, p<0.001), pain crises (OR=2.96, 95%CI:1.56-5.63, p<0.002), asthma (OR=2.46, 95%CI:1.38-4.36, p<0.003), headache (OR=2.44, 95%CI:1.04-5.7, p< 0.05), acute chest syndrome (OR=1.77, 95%CI:1.05-3, p<0.04), or priapism (male patients only, OR=6.48, 95%CI:1.59-26.42, p<0.01), in comparison to children with SCD without NDD. Children with SCD and NDD were more likely to have a history of hydroxyurea usage (OR=2.28, 95%CI:1.34-3.88, p<0.003), in comparison to children with SCD without NDD. Children with SCD and NDD had significantly higher odds of receiving school support (OR=9.34, 95%CI:4.68-18.64, p<0.001), in comparison to children with SCD without NDD.
Figure 1 shows the prevalence of reported NDD in this clinic population. Table 2 shows the different subtypes of NDD in this clinic population. The most common NDD were language disorders and ADHD. Four (18%) of the children with language disorders had been seen by a speech and language pathologist at the hospital. There was no significant difference in the odds of having a history of stroke between children with a history of SCD and a language disorder and children with SCD without language/other NDD (OR=3.3, 95%CI:0.97-11.18, p=0.055). ADHD had a prevalence of 7% in this SCD clinic population. Eleven (52%) of the children with ADHD had been seen by a behavioral therapist. Eighteen (86%) children with ADHD had been seen by either a neurodevelopmental physician or pediatric neurologist. Of the children with SCD and ADHD, 13 (62%) were on an appropriate medication for ADHD, either a stimulant medication alone (57%), alpha agonist alone (5%), or both (5%). Children with SCD and ADHD had higher odds of having a stroke in comparison to children with SCD without NDD (OR=7.42, 95%CI:2.55-21.58, p<0.001).
In conclusion, children with SCD and NDD have higher odds of having certain disease-related complications and higher use of disease modifying treatments than children with SCD who do not have NDD. The higher use of disease-modifying treatments could be due to the association of the NDD with SCD-related complications and the need to provide these children with a higher level of care. We cannot determine causal or temporal relationships between these NDD and SCD-related complications from this research. Screening and diagnoses of NDD may be relevant to clinical management of pediatric SCD.
Lance:NIH: Research Funding; KKI: Research Funding. Shapiro:HRSA: Other: Training Grant; Mutual Funds: Other: may invest in health care organizations; Baltimore City Health Department: Consultancy; Maternal and Child Health Bureau: Other: Training Grant. Casella:Immunoarray Ltd.: Patents & Royalties; Mast Pharmaceuticals: Consultancy; NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal