Background: Children with sickle cell anemia (SCA) are highly susceptible to stroke, impaired neurocognitive function and other manifestations of pediatric cerebral vasculopathy. Detailed multifaceted evaluations of children with SCA in sub-Saharan Africa are limited, including neurocognitive testing.
Methods: We aimed to establish the prevalence and types of neurocognitive dysfunction in a cross-sectional study in a randomly selected sample of patients with HbSS ages 1-12 years at a large SCD clinic in Kampala, Uganda. Neurocognitive function was assessed by Mullen Scales of Early Learning (ages 1-4) and Kaufman Assessment Battery for Children, 2nd edition (ages 5-12) using linguistically validated local translations (John CC, Pediatrics 2008; Bangirana P., Clin Infect Dis. 2014). The Behavioral Rating Inventory for Executive Function was used to assess executive function. Children also underwent standardized stroke examination (PedsNIHSS) and transcranial Doppler ultrasound (TCD) for measuring stroke risk by arterial velocities in pediatric SCD.
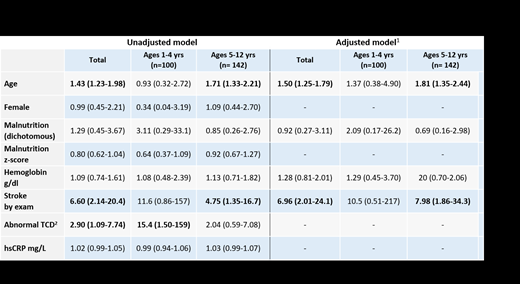
Results: Experienced testers performed neurocognitive assessment in 242 participants: 100 (41%) ages of 1-4 years and 142 ages 5-12 years (58.7%). Mean age was 5.44 ±2.9 years; 51.6% were male. Mean hemoglobin was 7.3 ±1.02 g/dl; 76.5% had hemoglobin <8.0 g/dl. Using established international standards, 16% were malnourished. In the older age group, more children were female, malnourished, and had a clinical evidence of a stroke. In all, 27 (11.2%) had neurocognitive dysfunction, and 63 (25.8%) with impaired executive function. In the 1-4 age group, 5 (5%) had an abnormal neurocognitive exam, with a lower average standardized Global Executive Functioning score (mean -1.70 (SD 0.78)) than in the overall neurocognitive testing. Dysfunction was more common in the group ages 5-12. Among the 5-12 age group, 22 children (15.4%) had overall neurocognitive dysfunction, with the lowest group average z-score being the standardized neurocognitive Global Executive functioning z-score (Mean -0.71, SD 0.84). In the overall sample, factors associated with neurocognitive dysfunction included age (OR 1.43, 95%CI 1.23-1.98), abnormal stroke examination (OR 6.60, 95%CI 2.14-20.4), and non-normal TCD (OR 2.90, 95%CI 1.09-7.74) (Table 1; bold font denotes significance at p<0.05). These results were consistent within the age subgroups. Adjusting for sex, hemoglobin, malnutrition and stroke, age (aOR 1.50, 95%CI 1.25-1.79) and stroke (aOR 6.96, 95%CI 2.01-24.1) remained significant predictors of neurocognitive dysfunction in the entire sample.
Conclusion: In children with SCA, executive function was the most common impairment. Overall, only 11% of the SCA children had impaired neurocognitive function. The major predictors of impairment were age, prior stroke and elevated TCD arterial velocity. These abnormalities were highly prevalent in the sample, and identifies significant disease-associated morbidity. Disease-modifying therapy should be assessed for improved neuropsychological function in these children.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal