Introduction: In the current era of comprehensive medical care in adults with sickle cell anemia (SCA), median survival is 48 years of age (Blood, 2019 Feb 7;133(6):615-617) with cardiopulmonary disease being a major cause of mortality. Despite lung disease being a major cause of death in young adults with SCD, no evidence-based guidelines are available to follow adults with SCD with pulmonary function tests (PFT). In addition to lung disease being a major cause of earlier death, we demonstrated forced expiratory in 1 second percent predicted (FEV1%) was associated with increased probability of premature death (hazard ratio per % predicted 1.02; 95% confidence interval [CI] 1.00-1.04; p=0.037) in a prospective cohort of young adults with SCA (n=430), with a mean age of 32.6 years (Blood, 2015 vol. 126(13) pp. 1544-50).
To provide additional evidence that lung function surveillance should be part of standard care for adults with SCD, we elected to compare the FEV1 volume loss in young adults with SCD to FEV1 volume loss in young adults with cystic fibrosis (CF). We selected CF because this disease is a well-established genetic disease where cardiopulmonary complications are the major cause of death. We tested the hypothesis that older adults with SCD (> 30 years of age) would have an absolute change per year in FEV1 similar to older adults with CF. If the results support the hypothesis, such a finding would provide additional evidence that monitoring decline in FEV1 in adults with SCD may lead to more targeted approaches for decreasing mortality.
Method: In a retrospective cohort study design conducted at Vanderbilt University Medical Center, we evaluated the electronic records of adults with SCD and CF. Individuals with either disease must have had at least 2 pulmonary function tests (PFTs) to be included. The absolute change in the FEV1 values was analyzed and compared between the groups. Adults with SCD received PFT evaluation at least once every two years as standard care. Only the first PFT in each year was used for adults with CF and evaluation could not be done within eight weeks of a hospital admission. A multivariable mixed model regression analysis was used to predict change over time in at least 2 spirometry evaluations with a pre-specified set of covariates previously associated with FEV1 decline in SCD or CF.
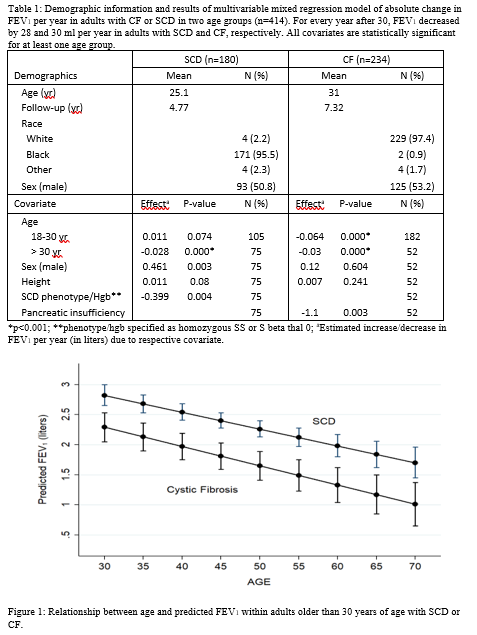
Results: A total of 180 and 234 adults with SCD and CF, respectively, with a mean age of 25.1 and 31.0 years, respectively, were included (see Table 1). The mean duration of follow up for adults with SCD and CF was 4.7 and 7.3 years, respectively. Using a multivariable mixed model regression analysis after adjusting for the statistically significant covariates (sex, SCD phenotype, and height for SCD; and sex, pancreatic insufficiency, and height for CF), the rate of FEV1 decline in individuals with SCD and CF over 30 years of age was 28 ml (p<0.001) and 30 ml (p<0.001) per year, respectively (p<0.001), These rates of decline were not different between the adults with SCD and CF (p=0.636), as shown in Figure 1. The rate of FEV1 change in individuals with SCD and CF between 18 and < 30 years of age was an increase of 10 ml per year (p=0.074) and a decrease of 64 ml per year (p<0.001), respectively (p=0.003).
Conclusion: Our results provide clear evidence that adults > 30 years of age with SCD have a rate of decline of FEV1 similar in magnitude to adults with CF greater than 30 years of age. Our new findings, coupled with our prior results indicating that lower FEV1% predicted was associated with earlier mortality in young adults with SCD, provide clear evidence that surveillance of FEV1 decline is warranted and therapeutic trials are needed if we are going to address all of the risk factors for attenuated life-span in adults with SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal