Background: The spleen is among the first organs negatively affected by sickle cell disease (SCD). Unswitched memory B cells (UMBCs) from the spleen, including the marginal zone B cells, circulate in peripheral blood and have been used as a measure of splenic function in non-hematologic disorders associated with functional asplenia. UMBC deficiency has been associated with adverse infectious and inflammatory outcomes in models of stroke and cardiovascular disease. The role of UMBCs has not been assessed in pediatric SCD. In this study, we sought to test he hypothesis that low UMBC is associated with significant infectious and inflammatory complications of SCD.
Design/Method: Children seen at the Texas Children's Cancer and Hematology Centers from March - December 2018 were recruited for participation. Participants were 18 months -18 years of age. Samples were collected for complete blood count, serum analysis, and B cell subset by flow cytometry. For B cell subset quantification, whole blood samples were stained with fluorescent-labelled CD45, CD19, IgD, and CD27. The samples were analyzed by flow cytometry using the BD LSR Fortessa or LSR II (BD Biosciences, USA). In each sample, at least 2500 CD19+ events were captured. Data were analyzed using FlowJo X.V. Clinical data was abstracted from the electronic medical record into an online study database. Statistical analyses were performed using STATA. This study was approved by the Baylor College of Medicine IRB.
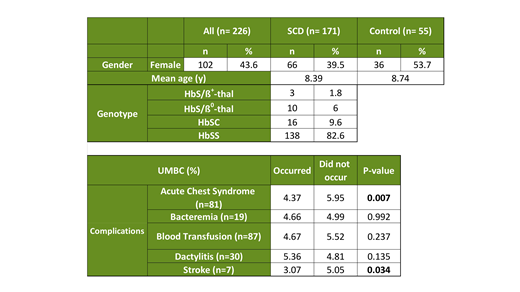
Results: We enrolled 234 subjects. Among these, 169 had an evaluable UMBC. Those with UMBC data included 114 (67.4%) Hb SS and Hb S/b0-thalassemia, 14 (8.3%) Hb SC, Hb b+-thalassemia, and HbS/other, and 41 (24.2%) controls without SCD. There was no difference in the mean age at sampling between children with SCD and controls without SCD (8.74 vs 8.39 years, P=0.70). The geometric mean UMBC was 5.75% of all CD19+ (B) cells for controls, 4.24 % for HbSS-like group, and 5.29% for SCD patients with any other genotype. UMBC declined by 2.97% per year among all SCD subjects (P<0.01). UMBC declined 0.82% per year among all controls, although the rate of decline was not significant, P= 0.62). The change per year did not significantly differ between cohorts (P=0.26).
To determine whether UMBC is associated with clinical complications of SCD, we reviewed the EMR of 127 subjects to identify any lifetime episodes of acute chest syndrome, bacteremia, blood transfusion, dactylitis, or stroke. Patients with any history of acute chest syndrome had significantly lower UMBC than those who have not had acute chest syndrome (median 4.3 vs. 6.2; P< 0.01). Patients with any history of stroke had significantly lower UMBC than those who have not had stroke (median 2.9 vs. 4.7; P=0.04). No significant difference was detected between groups with and without a history of bacteremia, blood transfusion, or dactylitis.
Conclusion: We have demonstrated that children with SCD are deficient in UMBCs and that UMBC deficiency worsens with age. UMBC deficiency is associated with history of acute chest syndrome and stroke. Additional studies are needed to establish the mechanisms of UMBC deficiency and the role of UMBCs in the clinical outcomes for children with SCD.
Tubman:Novartis Pharmceuticals: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal