Abstract
Background
ATG and post-transplant cyclophosphamide (PT-Cy) have been individually shown to be efficacious in reducing rates of GVHD in HLA matched and mismatched transplants. We adopted a combination regimen of ATG and PT-Cy for GVHD prophylaxis for matched unrelated donor (MUD) transplants in our centre to decrease the rates of acute and chronic GVHD.
Patients and methods
Pre-transplant conditioning consisted of iv Fludarabine (30mg/m2/day) for 4 days, iv Busulphan (3.2 mg/kg/day for 2 days), and low dose TBI (200cGy on day-1). GVHD prophylaxis was with Thymoglobulin 4.5mg/kg over 3 days (day-3 to -1), PT-Cy 50 mg/kg/day on days+3 and +4 and cyclosporine from day+5 (taper started by day+45 in patients without GVHD). The stem cell source was G-CSF stimulated peripheral blood stem cells (PBSC) in all patients.
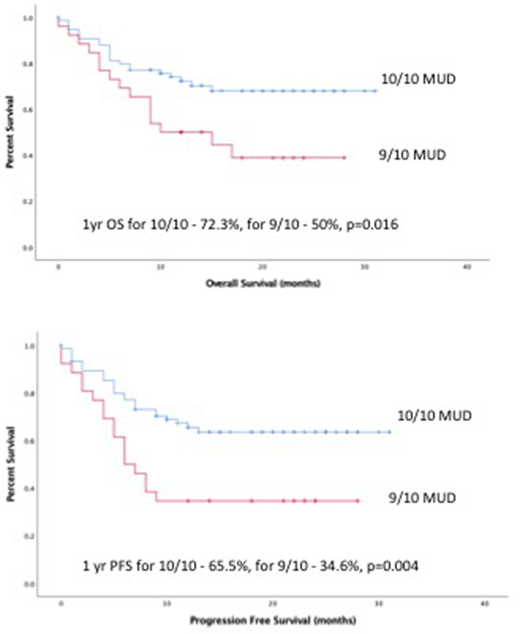
Overall survival (OS) and progression free survival (PFS) were calculated using Kaplan Meir method. Among variables included in Cox regression analysis to identify predictors of survival were age, pre-transplant remission status, occurrence of CMV infection, donor type (10/10 vs 9/10), and occurrence of acute or chronic GVHD.
Results
A total of 102 patients (median age 59y, range 22-74y) with high-risk hematological malignancies (AML-55, MDS-20, MPD-9, ALL-5, CML-4, lymphoma-6, CMML-3) were treated with this protocol. Unrelated donors were 9/10 matched in 26 patients, and the rest were 10/10 matched.
At a median follow-up of 12 months (range 0.5 to 31 months), the 1year OS and PFS were 66.5% (95% CI -57% -76%) and 57.6% (95% CI 47.6% -67.6%) respectively. The 1year OS for 10/10 transplants was 72.3% (95%CI 61.7%- 82.9%), which was significantly higher than that for 9/10 transplants at 50% (95%CI 30.4%- 69.6%, p=0.016). The 1year PFS for 10/10 donor transplants was 65.5% (95% CI-54.3%- 76.7%) which was significantly higher than that for 9/10 transplants at 34.6% (95%CI 16%- 53.2%, p=0.004). The 9/10 matched patients had significantly higher relapses (hazard ratio 3.2, 95%CI 1.4-7.1, P=.005) than 10/10 matched patients.
There were five graft failures (one primary and four secondary). The non-relapse mortality (NRM) was 17.6 %. The overall incidence of acute GVHD was 40% (grade 3-4 acute GVHD was seen in 14.8% patients). The overall incidence of chronic GVHD was 19.6% (moderate/severe NIH stage chronic GVHD was seen in 8.8% patients). The overall relapse rate was 23.3%. CMV re-activation was seen in 50 (49%) patients, and EBV re-activation in 20 (19.6%) patients, and 10 (9.8%) patients were diagnosed with post-transplant lympho-proliferative disorder (PTLD).
In univariate analysis, adverse predictors of survival were a) persistent disease at the time of transplant, b) absence of chronic GVHD, and c) 9/10 donor type. In multivariable analysis, the only independent predictors of survival were a) persistent disease at time of transplant [hazard ratio 6.96, 95% CI 1.97-24.7, p=0.003], and b) donor type 9/10 vs 10/10 [HR 2.59, 95% CI 1.15-5.8, p=0.022].
Conclusion
Our experience shows that PT-Cy and ATG can be combined for GVHD prophylaxis in MUD PBSCTs with low rates of Gr3-4 acute GVHD and chronic GVHD, and acceptable NRM and relapse rates. There were high rates of viral reactivation including PTLD.
Lipton:ARIAD: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal