Abstract
INTRODUCTION: Cardiac involvement is common in both wild-type transthyretin (wATTR) and AL amyloidosis and these entities can have overlapping clinical features (Banypersad et al, JAHA 2012). Accurate diagnosis is vital given differences in spectrum of disease, management, and prognosis. We examined the presenting clinical features and survival outcome of patients diagnosed with cardiac wATTR and AL amyloidosis confirmed by mass spectrometry.
MATERIALS & METHODS: Patients diagnosed between January 2014 and September 2017 with biopsy proven wATTR or AL amyloidosis and cardiac involvement by consensus criteria (Gertz et al, Amyloid 2010) were included. Mass spectrometry testing was performed at the Mayo Clinic Laboratories to confirm amyloid subtype in all cases. Patient records were retrospectively reviewed to identify clinical characteristics as well as details regarding treatment and survival.
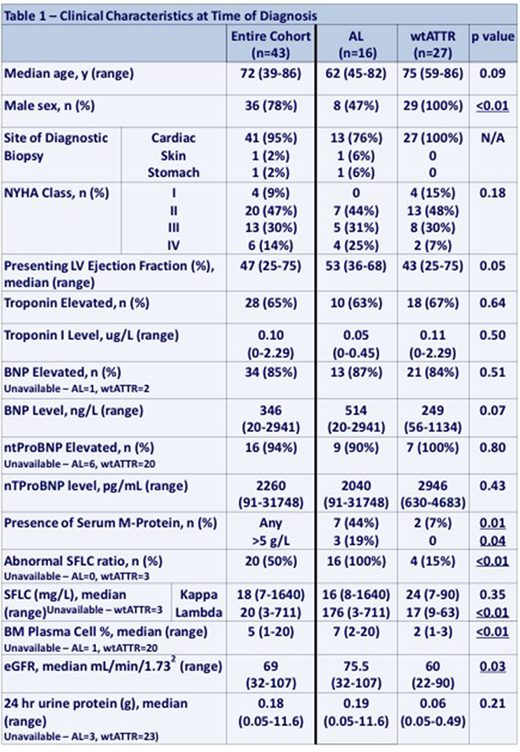
RESULTS: Forty-three patients were identified (wATTR n=27, AL n=16) with site of biopsy: 41 cardiac (95%); 1 gastric (2%); 1 skin (2%). Two (13%) patients with AL amyloid had coexisting multiple myeloma. Thirty-five (81%) patients were male, with a strong male predominance in wATTR patients (100% vs 50% for AL patients, p=<0.01). Median age at diagnosis was 73 years (range 45-86), with a trend towards older age in wATTR patients (median 75 vs 62 years for AL patients, p=0.09). No difference was seen in presenting NYHA class or levels of troponin and ntProBNP between amyloid subtypes. BNP trended towards higher values in AL patients (median 514 vs 249 ng/L for wATTR, p=0.09). wATTR amyloid patients had lower median presenting left ventricular ejection fraction (43 vs 53%, p=0.05). Two (7%) patients with wATTR amyloid had an M-protein on SPEP compared to 7 (44%) with AL amyloid. Only 2 patients with AL amyloid had M-protein greater than 5 g/L while both wATTR patients had less than 5 g/L. In those with serum free light chain testing available (wATTR n=24, AL n=16), median lambda light chain level was higher in AL patients (176.0 vs 16.9 mg/L for wtATTR, p=<0.01). No difference was seen in kappa light chains (16.5 vs 23.8 mg/L for wATTR, p=0.60), though the only patient with kappa AL amyloid had kappa light chains significantly elevated at 1640 mg/L. The kappa/lambda ratio was abnormal in 15% of wATTR patients (all kappa predominant) compared to 100% in AL amyloid patients (94% lambda predominant) (p=<0.01). The median difference between involved and uninvolved light chain (dFLC) was 22 mg/L for wtATTR patients compared to 249 mg/L for AL patients. In patients with bone marrow biopsy results available (AL n=15, wATTR n=7), bone marrow plasma cell percentage was higher in patients with AL amyloid (median 7% vs 2%, p=0.01). No monoclonal plasma cells were seen on bone marrow in wATTR patients by immunophenotype.
Treatment for patients with AL amyloid was: bortezomib, cyclophosphamide, and dexamethasone (VCD) in 11 (69%); VCD followed by melphalan 200 mg/m2 autologous transplantation in 1 (6%); melphalan/dexamethasone in 1 (6%); no treatment in 2 (13%); unknown in 1 (6%). In evaluable patients, hematologic response rate was 54% (complete response n=4, very good partial response n=2, partial response n=1, no response n=6). With a median follow-up of 1.8 years for surviving patients, 1 year overall survival (OS) was 76% for the entire cohort. Patients with AL amyloidosis had significantly poorer 1 year OS (41% vs 92% for wATTR patients, p=<0.01). Patients with NYHA class 3-4 had significantly worse 1 year OS (54% vs 96% for those 1-2, p=<0.01), and this held true for both AL and wATTR patients. In AL patients, revised Mayo stage (Kumar et al, JCO 2012) of III-IV predicted for poor 1 year OS (19% vs 75% for stages I-II, p=0.03), as did not achieving complete response to primary treatment (1 year OS 33% vs 67% for CR patients, p=0.06).
DISCUSSION & CONCLUSIONS: Male sex, older age, and lower LVEF were more common in patients with wATTR compared to AL amyloidosis. Higher levels of BNP, larger dFLC with lambda predilection, and higher bone marrow plasma cell percentage were more common in AL amyloid patients. Overall survival was significantly worse for patients with AL amyloidosis, particularly those with high NHYA class, advanced revised Mayo stage, and suboptimal response to primary therapy. These results highlight the importance of accurate amyloid sub-typing in patients with suspected cardiac amyloidosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal