Abstract
Introduction: Mucopolysaccharidosis Type I (MPS-I) is a lysosomal storage disease resulting in progressive multisystem involvement and ultimately death at a young age. Since 1980, hematopoietic stem cell transplant (HSCT) has been used to treat MPS-I and stabilize cognitive impairment. However, little is known regarding overall outcomes and healthcare utilization of HSCT compared to enzyme replacement therapy (ERT) versus other supportive treatments.
Method: We utilized the Pediatric Health Information System, a validated multi-institutional pediatric and adolescent database from 45 individual pediatric institutions, to identify and analyze patients diagnosed with MPS-I between 2005 and 2017. A retrospective analysis was performed to examine outcomes and healthcare utilization between three cohorts: patients who received HSCT at less than one year old, patients who received HSCT at greater than one year old, and patients who did not receive HSCT.
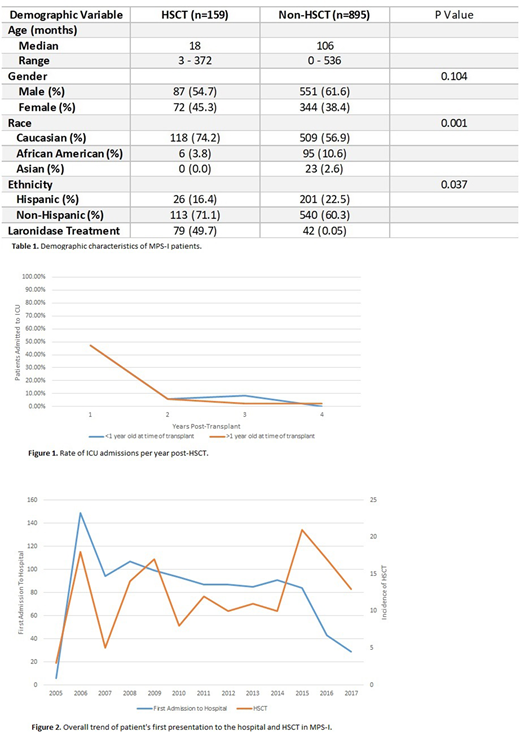
Results: In the largest reported cohort of 1,053 patients identified with MPS-I, approximately 15% received HSCT while others received ERT alone or supportive treatments. Approximately 23% of patients received HSCT at less than one year of age with the remainder of patients received HSCT at greater than one year of age (Table 1). There was no difference in incidence of acute graft versus host disease (GHVD) (p=0.980) between the younger (25.0%) and older (25.2%) transplant cohorts. In our sample, 12.2% of patients who received HSCT after one year of age were diagnosed with chronic GVHD in comparison to 5.6% of the younger cohort (p=0.364). There was no difference in likelihood of ICU admission when comparing non-HSCT management (53.9%) to both the younger (52.8%) and older (61.0%) HSCT cohorts (p=0.899, p=0.138 respectively). In both transplant cohorts the greatest likelihood of ICU admissions occurred during the first year post-transplant, after which the rate plateaued (see Figure 1). Infection was the most common reason for hospital admission among all patients, with severe infection being more common in both the younger HSCT cohort (OR 2.58, CI 1.32-5.04) and older HSCT cohort (OR 2.38, CI 1.62-3.49) when compared to non-HSCT management. When analyzing mortality between all cohorts, non-HSCT patients had a lower rate of mortality compared to patients who received HSCT at an older age (OR 3.50, CI 2.00-6.14). However, we found no difference in mortality between non-HSCT patients and HSCT at less than one year old (p=0.426). Approximately 50% of HSCT patients received ERT; we found no difference in overall survival between patients who received ERT and those who did not (p=0.796). Figure 2 shows the trend of MPS-I patients' first presentation to the hospital plotted alongside the incidence of HSCT in our sample between 2005 and 2017. When looking at the incidence of HSCT in relation to new presentations of MPS-I, a higher proportion of patients received HSCT during 2012-2017 (18.9%) as compared to 2005-2011 (12.6%) (p=0.005).
Conclusion: When considering HSCT as treatment for MPS-I, HSCT at a younger age is associated with increased overall survival. This study found that ERT in addition to HSCT had no effect on overall mortality. The lack of difference between transplant and non-transplant ICU admissions indicates that HSCT does not significantly contribute to overall ICU admissions. Likelihood of ICU admission plateaus after one year, regardless of age at transplant. Infection is the most common reason for hospital admission for all patients with MPS-I diagnosis, however severe infection is more common among HSCT patients when compared to non-HSCT patients. First presentations to hospitals have down trended over the past several years while the number of HSCT each year has remained relatively stable, resulting in an increased proportion of HSCT incidence to new MPS-I presentations in hospital settings. One possible explanation is the recent implementation of newborn screening, which provides earlier detection of the disease. This may allow outpatient management at a young age and potentially avoid MPS-I manifestations resulting in hospital admissions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal