In this issue of Blood, Amin et al provide data showing early compression therapy post–venous thromboembolism (VTE) to be effective in reducing the incidence of postthrombotic syndrome (PTS) by achieving reduced residual vein obstruction (RVO) on follow-up ultrasound.1
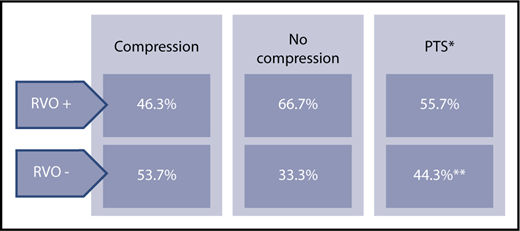
Results summary. Asterisk (*) indicates measured at 6 months. Double asterisks (**) indicate odds ratio, 0.66; 95% confidence interval, 0.46-0.96.
Results summary. Asterisk (*) indicates measured at 6 months. Double asterisks (**) indicate odds ratio, 0.66; 95% confidence interval, 0.46-0.96.
PTS is a significant, disabling,2 and costly3 complication in up to 50%4 of patients with VTE. Given that other PTS treatment interventions, such as the use of elastic compression stockings,5 or early thrombolysis6 provide limited benefit or are controversial in reducing the incidence of this morbidity, the current findings are potentially of great clinical interest. The scale of benefit appears comparable to the effect of well-controlled anticoagulation therapy on risk reduction of the incidence of PTS.7
Variable in incidence, and in severity, PTS is a common and potentially disabling longer-term complication of deep vein thrombosis (DVT). Symptoms can range from pain, swelling, skin changes, and heaviness of the limb to venous claudication and development of venous ulcers in the most severe cases. The cost in terms of medical care and loss of quality of life are well documented and considerable.1-4 The impact of PTS on health is comparable to that associated with major chronic diseases.2,3 Prevention of the development of PTS should be optimized, as treatment options for symptom control are of limited benefit. Standardized diagnostic criteria, and clinical risk factors associated with the occurrence of PTS are now better understood.4,5 The pathophysiology of PTS is thought to be related to venous hypertension and its detrimental effects on vascular integrity, venous insufficiency, and the inflammatory response.4 Clot burden and vein obstruction are associated with venous hypertension. Residual vein obstruction as evaluated on follow-up ultrasound is associated with the risk of PTS.8 Efforts to reduce clot burden and obstruction by means of early thrombolysis or interventional stents and recanalization procedures have shown success in reducing PTS in some patients.6 Both approaches are, however, invasive, associated with potential complications, and depend on specialized resources. Amin et al have used a simple, noninvasive treatment, early external compression by bandages or stockings applied 24 hours post-DVT diagnosis, for a duration of 4 weeks. Their data show a 20% absolute risk reduction in the incidence of residual vein obstruction measured 1 week prior to discontinuing anticoagulation. The benefit of vein recanalization also translates to an 11% absolute risk reduction in the development of PTS measured at 6 months post-DVT diagnosis (see figure).
These findings thus corroborate the pathophysiologic role of residual clot in the development of PTS and provide data to suggest that a simple, noninvasive treatment intervention of early compression has a role in promoting clot resolution and reducing the incidence of postthrombotic complications. The use of early compression was not randomized in this study but reflected local practice. Anticoagulant treatment was mostly with vitamin K antagonists but did include the use of low-molecular-weight heparin and direct oral anticoagulants in the minority of the study patients. Anticoagulation control was optimal for both early compression and noncompression groups. All patients subsequently wore elastic compression stockings for a minimum of 6 months. The 2 patient groups did differ in some baseline characteristics, which were adjusted for on statistical analysis. A subgroup analysis of patients with ileofemoral DVT showed a lack of therapeutic effect in the compression group, thus remaining a challenging patient population for PTS prevention. The large sample size and long-term follow-up of the overall patient group strengthen the conclusions of the current study.
The simplicity of the early compression should make this intervention easily available in all health care institutions and should be strongly considered for implementation. Further studies to refine the application and risk stratify patients for greatest potential benefit, along with the evaluation of other interventions to reduce the incidence of PTS, are awaited with interest.
Conflict-of-interest disclosure: The author declares no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal