Abstract
Background
Bleeding disorders in women are under-recognized and under-treated. Women are equally as likely as men to have bleeding disorders other than hemophilia and are disproportionately affected by these diseases due to the bleeding challenges of menstruation and childbirth. The most common bleeding disorder identified in women is von Willebrand disease (VWD). Heavy menstrual bleeding (HMB) is the most common symptom in women with VWD, occurring in up to 93% of patients. Among women with HMB, the reported prevalence of VWD ranges from 5─20%. Women with VWD are also more likely to be diagnosed with hemorrhagic ovarian cysts due to ovulation-associated bleeding and endometriosis due to increased retrograde menstruation. As a result, women with bleeding disorders are more likely to undergo hysterectomy and also undergo hysterectomy at an earlier age than women without bleeding disorders. In 2001, the American College of Obstetrics and Gynecology (ACOG) recommended VWD screening prior to hysterectomy in women with HMB. The actual frequency of VWD screening in clinical practice is unknown.
Objectives
In this study, we assess patterns of VWD screening in a nationally representative sample of women undergoing hysterectomies for HMB.
Methods
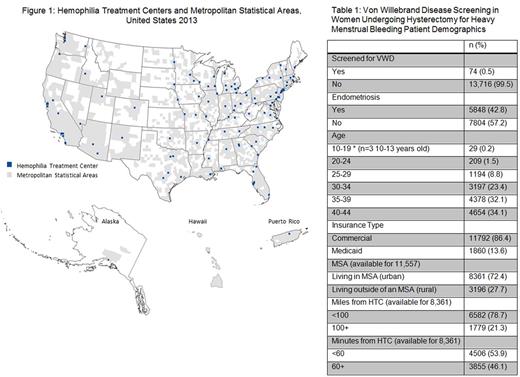
We used the Truven Health MarketScan® Research Databases which include the medical prescription claims of over 109 million covered lives as well as Medicaid data on 8.6 million patients from 14 states. The MarketScan Databases contain patient demographics, physician and facility claims and pharmacy claims. Procedure codes were used to identify women ages 10-44 years undergoing hysterectomy or hysterectomy alternative (HA) from 2011-2013. Subjects were required to have 12 months of continuous enrollment prior to surgery date. We utilized ICD-9 codes to categorize hysterectomy indications and only included women with a diagnosis of excessive bleeding as the indication for surgery. Women with fibroids, genital tract malignancy, and previously diagnosed bleeding disorders were excluded. We defined VWD screening as a laboratory claim for either VWF:Antigen and/or VWF:Activity within the 12 months preceding hysterectomy. To determine if patient and facility level characteristics impacted access to specialty hematology care and/or screening for VWD, we collected the following information: 1) known bleeding disorder diagnosis and/or endometriosis prior to surgery; 2) age; 3) whether patient was living in metropolitan statistical area (MSA; used as a surrogate marker for urban vs rural inhabitance); 4) number of miles and approximate travel time to nearest Hemophilia Treatment Center (HTC). We used ArcMAP® software to calculate distance between the MSA and nearest HTC. MSA data was only available for commercially-insured patients. (Figure 1) Logistic regression was used to assess factors related to the occurrence of VWD screening.
Results
We identified 13,790 women who underwent hysterectomy/HA for HMB. We excluded 138 with known bleeding disorders leaving 13,652 women in our final analysis (Table 1). Of these, 74 (0.5%) were screened for VWD within 12 months preceding surgery. There were 2,000 women (15%) who underwent other coagulation tests, most commonly prothrombin time and partial thromboplastin time. We had MSA data on 11,557 commercially-insured women, of whom 72.4% lived within a MSA. Women living in a MSA were screened more often than those outside of a MSA (p=0.013). For those living within a MSA, the odds of being screened for VWD was lower in women with endometriosis (OR=0.54, 95% CI 0.31, 0.97; p=0.038) and women living >100 miles from the nearest HTC (OR=0.29, 95% CI 0.11, 0.81; p=0.017).
Discussion
This study demonstrated that despite ACOG expert recommendations, the frequency of VWD screening in a nationally-representative population of publically and commercially-insured women undergoing hysterectomy for HMB was very low. Greater distance from a HTC or a prior diagnosis of endometriosis further reduced the likelihood of VWD screening. It is important to increase awareness that a diagnosis of endometriosis does not rule out the presence of a bleeding disorder. This study brings to light the need for the hematology community to improve education and awareness among women's health providers in order to identify women with bleeding disorders and allow for optimal medical management of HMB prior to surgical consideration.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal