Abstract
Background
Various imaging techniques are used for management of patients with multiple myeloma (MM) after Autologous Stem Cell Transplantation (ASCT). Between them, PET-CT is a whole-body, high-sensitive imaging tool used to discriminate bone involvement. About the prognostic role of PET-CT, the NCCN guidelines state that "PET-CT results after induction therapy and stem cell transplant help in predicting prognosis of patients with symptomatic MM". Several previous studies demonstrated that the presence of at least 3 focal lesions with SUV>4.2 and extra-medullary disease was associated to shorter PFS and OS [Zamagni E, 2011]. With these premises, we decided to retrospectively assess if PET-CT precociously performed after ASCT (at 3-6 months) would be able to predict the quality of response or survival in our series of autotransplanted MM patients.
Methods
45 patients underwent to PET-CT after ASCT: two third of them received as induction the combination of bortezomib, thalidomide, and dexamethasone (VTD); another quarter received bortezomib, anthracycline, and dexamethasone (VAD); the remaining subjects were treated with bortezomib or thalidomide and dexamethasone (VD, TD).
Results
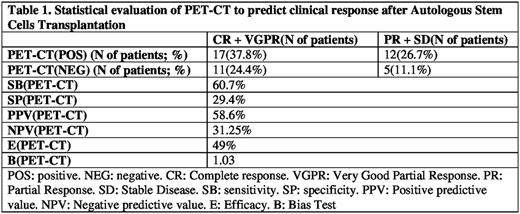
The 67% of patients receiving VTD as induction achieved a response, with 69% of CR+VGPR versus the only 7% of optimal responses offered by the VAD regimen. At the end of the high-dose procedure, overall 62% of our patients were in CR o VGPR. The median OS was 58 months, and at 40 months the 45% of our patients was still progression-free. In order to avoid positive and negative falses, we calculated the specificity and the sensitivity of PET-CT: in our hands, PET-CT sensitivity resulted 60.7% and specificity 29.4%. For further details, see Table1.The PET-CT positivity did not significantly correlate with the clinical response assessed at the same time-points: indeed, in the subgroup of PET-CT-positive cases, the 26.7% showed a poor response, as expected. Nevertheless, unexpectedly, the 37.8% of positive cases achieved at least a VGPR. On the other hand, the 24.4% of cases with negative PET-CT were in good response, but, conversely, 11.1% of these PET-negative patients were in poor response (p=ns). Overall, the median OS was 17 months in PET-CT-positive patients versus not reached at 40 months in the negative subgroup; nevertheless, this difference was not statistically significant (p=0.29). Finally, we assessed if PET-CT status after ASCT could predict the OS length: in this setting, the median OS was 23 months for PET-CT-positive patients versus not reached at 40 months in the negative subgroup; even in this case, this difference was not statistically significant (p=0.28). The same analysis was performed in terms of PFS: overall, the median PFS was 18 months in PET-CT-positive patients versus 37 months in the negative subgroup; (p=0.55). Finally, we assessed if PET-CT status during follow-up could predict the PFS length: the median PFS of the entire series was 32 months for PET-CT-positive patients versus 60 months in the negative subgroup; once more, this difference was not statistically significant (p=0.15).
Conclusions
In conclusion, the status of PET-CT precociously performed after ASCT was not able to discriminate quality of response or survivals in our patients. This result does not confirm already published data; we argue that this discrepancy could depend on the adoption in our series of the newer and more effective regimens in respect of the VAD, previously adopted in the studies where a significant prognostic impact of PET-CT was demonstrated. Finally, another relevant aspect of our study is that it represents the output of a real-life experience.
Galimberti: Novartis: Speakers Bureau; Pfizer: Speakers Bureau; Bristol-Myers Squibb: Speakers Bureau; Incyte: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal