Abstract
We present a unique case of sickle cell disease with variant C antigen and multiple alloantibodies including Anti-Dombrock a (Doa) that presented as a challenge in transfusion management.
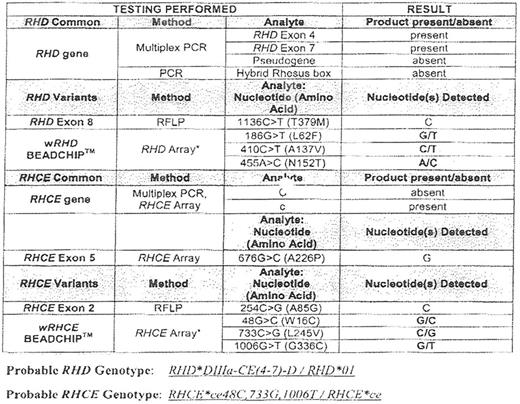
A 20-year-old female sickle cell patient is on multiple and frequent transfusions (~25/year). She has a history of anti-Fya, anti-C, anti-K, anti-S, anti-M, anti-Lea, and warm autoantibodies. Recently, she presented with anti-C alloantibody even though she was C antigen positive by antisera testing, so genotyping was done. The 3 nucleotide substitutions detected in the RhD gene (186G>T, 410C.T, 455A>C) and the RhCE gene (48G>C, 733C>G, 1006G>T) constituted a genotype of Dce/Cvarepar and a predicted phenotype of D+altered C+E-c+e+VS+V-hrB+.
She has also developed indirect antiglobulin testing reactivity that 'comes and goes' despite being given phenotype matched blood. The reactivity that comes and goes was identified as Anti-Doa using the Doa negative genotype and an extended antibody ID panel.
Some variant C antigens act as partial C antigen, thus, these patients may make anti-C alloantibody. The frequency of Doa antigen is 66.7~55% depending on race, but reagent antisera for Doa antigen is not commercially available yet. Anti-Doa can disappear in vivo but can cause delayed and acute/hemolytic transfusion reactions. We have been giving her genotype matched blood. Such a patient with multiple RBC antibodies on chronic transfusions presents as a challenge in transfusion management that mandates extensive testing. The extensiveness of the pretransfusion testing in these patients is left to the individual pathologist's decision.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal