Abstract
The recently implemented Oncology Care Model (OCM)-a demonstration project by CMS and alternative to fee-for-service reimbursement in traditional Medicare-is intended to reduce inefficient spending for the treatment of cancer patients. The OCM rewards practices whose total Medicare spending per episode falls below a threshold set to yield savings to the Medicare program. For example, under one version of the OCM, practices can receive a performance-based payment if spending per episode falls below a threshold that is 4% lower than projected spending under existing trends.
In this study, we investigate two questions related to the potential impact of the OCM on hematology practices compared to practices that focus on solid tumors. First, is the level of spending in OCM-defined episodes greater for hematologic cancers? If so, larger dollar reductions per episode must occur for hematology practices to meet the percentage reductions required for receipt of performance-based payments. Second, does the distribution of episode spending by service category differ substantially between hematologic and solid tumor cancers? If the fraction of spending on categories such as inpatient hospital care and imaging-which are often viewed as sources of savings through better care management-is smaller for hematologic cancers and the fraction of spending on chemotherapy- which directly treats the disease-is greater, then hematology practices may find it more difficult to stay within OCM thresholds.
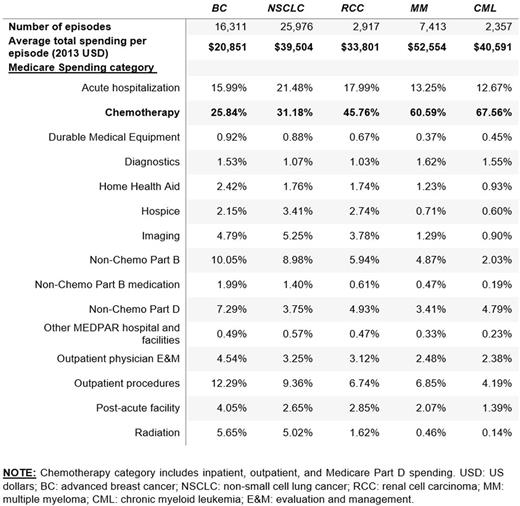
To address these questions, we examine the distribution of total spending in hypothetical OCM episodes for 5 cancers: two hematologic (chronic myeloid leukemia (CML) and multiple myeloma (MM)), and three solid tumors (advanced (stage 3 & 4) breast cancer (BC), non-small cell lung cancer (NSCLC), and renal cell carcinoma (RCC)). Using SEER-Medicare data from 2007-2013, we constructed an episode-level dataset following the OCM definition of a treatment episode, namely, 6 months beginning with the onset of outpatient chemotherapy treatment, either infused or oral.
Total health care spending was calculated for each episode, and every claim within an episode was assigned to a subcategory of spending (eg. inpatient hospital care, chemotherapy, imaging, lab, and so forth).
For the period 2007-2013, overall mean per-episode spending ranges from $20,851 in BC to $52,489 in MM (see table). Hematologic cancers were more expensive overall per episode than BC, RCC, and NSCLC. In all 5 cancers, the largest contributor to overall spending was chemotherapy (including inpatient, outpatient, and Part D claims). Approximately two-thirds of episode spending in CML and MM is for chemotherapy (68% and 61%, respectively), whereas chemotherapy constitutes only 26% of BC spending, 31% of NSCLC spending, and 46% of RCC spending. Acute hospitalization, the next largest contributor to overall episode spending, constitutes a larger share in BC, RCC, and NSCLC (16%, 18% and 21%, respectively) than MM and CML (13% in both). Spending in many subcategories tends to be a smaller share of overall spending for hematologic cancers; examples include imaging, outpatient physician evaluation and management (E&M), and hospice.
These data demonstrate that hematologic cancer treatment is more costly than solid tumor treatment during episodes as defined under the OCM, implying that a greater dollar amount of savings per episode must be obtained for hematology episodes under the OCM in order to qualify for performance-based payments. Furthermore, the data show that hematology episodes have less room for obtaining savings from typical management targets such as inpatient care and imaging, suggesting that hematology practices will find it more difficult to stay within OCM thresholds. These results represent only a sample of tumor types, but suggest a more extensive examination of spending is needed to determine whether these results generalize to a larger set of cancers. If the much larger fraction of spending for chemotherapy for CML and MM extends to a broader set of hematologic malignancies, hematology practices will face more financial pressure to reduce spending on chemotherapy than non-hematology practices. Refinements in the OCM and similar innovative payment models may be necessary in order to avoid unintended consequences for patients with hematologic malignancies.
Baumgardner: Precision Health Economics: Employment. Shahabi: Precision Health Economics: Employment. Linthicum: Precision Health Economics: Employment. Vine: Precision Health Economics: Employment. Zacker: Novartis: Employment, Equity Ownership. Lakdawalla: Precision Health Economics: Consultancy, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal