Abstract

Introduction
Allogeneic hematopoietic stem-cell transplantation (AHSCT) is an effective treatment for patients with high-risk or relapsed acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS). Several factors are known to influence survival post-transplant. Our group developed a model to predict survival in a small number of patients with AML/MDS using 3 disease (cytogenetics and disease status at transplant) and patient-related [Hematopoietic stem cell transplant comorbidity index (HCT-CI)] variables (Bachegowda et al.Blood.2017) . This model effectively stratified AML/MDS patients into 3 risk groups with very different survival. Here we aim to validate this model in a large cohort of AML/MDS patients receiving AHSCT with various donor types.
Methods
A total of 934 patients with AML/MDS consecutively treated at the University of Texas MD Anderson Cancer Center were included in this analysis. Donors were HLA matched related (n=377, 40%), matched unrelated (n=416, 45%) mismatched unrelated (n=68, 7%) and T-cell replete haploidentical transplants (n=73, 8%). The median age was 53 years (range 18-65 years). Cytogenetics data at diagnosis was available in 920 patients and was favorable, intermediate and adverse-risk in 340 (37%), 517 (56%) and 63 (7%), respectively. Five hundred and forty patients (58%) were in first or second complete remission (CR1/2). The hematopoietic stem cell transplant comorbidity index (HCT-CI) was available in 914 patients and the median score was 2 (range 0-17). The sources of hematopoietic stem cells were peripheral blood for 586 patients (63%) and bone marrow for 348 patients (37%). Seven hundred and eighty patients (84%) received myeloablative-conditioning chemotherapy.
Results
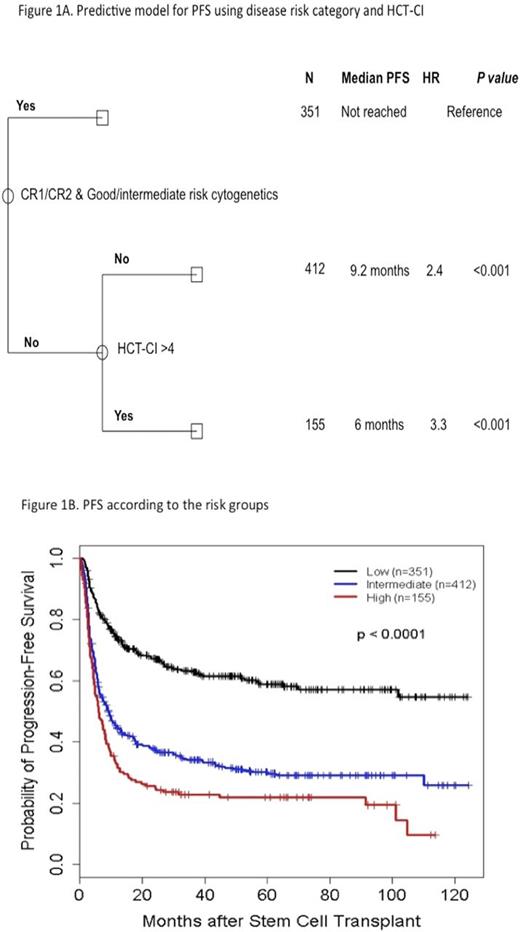
Patients were stratified into 3 risk groups according to the previously published model: 1) low-risk group (patients in CR1/2 with intermediate/favorable risk cytogenetics, irrespective of HCT-CI (HCT-CI did not impact survival in this group) (n=351), 2) intermediate-risk group (patients beyond CR1/2 and/or with adverse-risk cytogenetics and HCT-CI score ≤4) (n=412), and 3) high-risk group (patients with at least one negative prognostic factor - beyond CR1/2 and/or with adverse-risk cytogenetics and a HCTCI score >4) (n=155).
Median follow up duration for 436 survivors was 48 months. For the whole group, the 5-year progression-free survival (PFS), treatment-related mortality (TRM) and relapse rate were 39%, 21% and 39%, respectively. TRM at 5 years for low-risk group was 17%, for the intermediate-risk group was 18% (HR [95% CI] 1.12 [0.79-1.59]; P=0.52), and for the high-risk group was 40% (3.24 [2.26-4.64]; P<0.0001), respectively, whereas cumulative incidence of relapse at 5 years was 24% for low-risk, 52% for intermediate-risk (2.86 [2.20-3.71]; P<0.0001) and 38% for the high-risk group (1.88 [1.34-2.63]; P<0.0001), respectively. In multivariable model, transplantation in >CR1/2 (2.84 [2.38-3.40]; P<0.0001), adverse cytogenetic risk (1.54 [1.29-1.83]; P<0.0001), males (1.23 [1.03-1.46]; P=0.022) were significantly associated with worse PFS while higher age-adjusted HCT-CI scores (1.20 [0.99-1.47]; P=0.06) approached significance. Other factors including conditioning intensity (1.02 [0.82- 1.29]; P=0.84, age (1.01 [1.00-1.01]; P=0.17) and donor type (haploidentical (1.2 [0.83-1.72]; P=0.33), matched unrelated (1.06 [0.88-1.28]; P=0.55) and mismatched unrelated donor (1.07 [0.76-1.50]; P=0.70) as compared with matched related donor) did not significantly influence PFS. Using our previously described predictive model, the patients separated in 3 risk groups with significantly different median PFS, which was not reached for the low-risk group, 9.2 months for the intermediate-risk group (2.4 [1.97-2.99]; P<0.0001), and 6.0 months for the high-risk group (3.3 [2.57-4.21]; P<0.0001), respectively. (Figures 1A and 1B)
In conclusion, we were able to stratify allogeneic stem cell transplant patients in 3 risk groups based on a combination of disease (cytogenetics and disease status at transplant) and patient-related factors (HCT-CI) with significantly different survival. HCT-CI appears to have a much higher discriminatory impact in patients with higher risk disease (not in CR1/CR2 and/or adverse risk cytogenetics) compared with those in the lower risk group (CR1/CR2 and intermediate/favorable risk cytogenetics).
Oran: AROG: Research Funding; Celgene: Research Funding; Astex: Research Funding. Khouri: Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal