Abstract
Background
Several groups have reported use of haploidentical peripheral blood donor cells as adjunct to chemotherapy in remission induction of myeloid leukemia (Colvin et al, BBMT 2009, Gue et al, Blood 2011). Moreover, CB grafts have been associated with greater disease control and enhanced graft-versus-leukemia responses, as a consequence of the fetal-maternal interactions during pregnancy (van Rood et al, PNAS 2009 and PNAS 2012).
We evaluated prospectively the feasibility and tolerability of infusing partially HLA matched cord blood units (CBUs) with specific alloreactive properties after salvage chemotherapy to patients (pts) with refractory myeloid leukemia.
Patients and Methods
Pts with confirmed diagnosis of AML or MDS, according to WHO classification (excluding acute promyelocytic leukemia) who had received two or more previous induction/re-induction regimens were eligible. All pts were treated at NYPH and all CBUs were obtained from the NCBP. The study was performed under FDA IND and was approved by the IRBs of both institutions. Pts received induction chemotherapy followed by CBU infusion (1-3 days later) without any immunosuppression.
CBUs eligible for the study contained a pre-cryopreservation Total Nucleated Cell (TNC) dose of 0.5-2.5x107/kg. They were HLA matched at 4-6/6, HLA-A, -B intermediate resolution, -DRB1 high resolution. CBUs had undergone HLA typing of the mother, thus allowing determination of the paternal and maternal antigens. CBUs with shared IPA targets and/or NIMA match were selected for cell therapy.
Results
A total of 34 patients underwent CBU search. Mean CBU number per search was 134 (range: 7-250) with 58% potentially eligible CBUs per pt (range: 5-159). A total of 143 CBUs underwent testing including HLA confirmatory typing. At least one eligible CBU was identified for each pt. Higher HLA allele level match was preferred in the final selection.
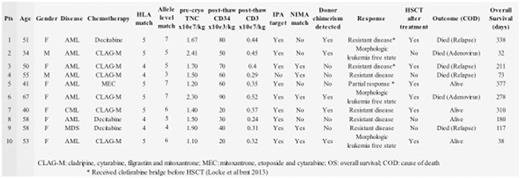
Of the 34 pts, 23 did not receive treatment because of progressive disease and death (n=8); other clinical trials/treatments (n=6); hematopoietic stem cell transplants (HSCT) (n=9); while one is currently undergoing evaluation. Ten pts have been treated (Table); 8 had AML, 7 with primary induction failure (PIF); one had myeloid blast phase CML and one with high risk MDS. Nine pts had poor risk karyotype and 4 had prior allografts. Median age was 52 years (range: 34-67); median number of prior treatments was 11 (2-15) and median HSCT-CI was 3 (0-7).
Of the CBUs infused, six were 5/6 and four were 4/6 HLA matched. The allele level compatibility and presence of shared IPA targets and/or NIMA matches are shown in the Table. CBU median TNC was 90x107 (range: 63-151) and they tended to be "older" with a median cryopreservation time of 10 years. CBUs provided a mean cell dose of 1.66 x 107 TNC/kg (range: 1.1-2.4). Mean post-thaw CD34+ and CD3+ cell doses were 52x103/kg (range: 20-90) and 0.34x107/kg (range: 0.24-0.52; SD: 0.08), respectively, with excellent post-thaw CD34+ viability (93.5%-98.3%).
No CBU infusion reactions or cytokine release syndrome were observed. One pt, recipient of a prior allograft with no history of GVHD, experienced skin rash 1 week after CBU infusion. The skin biopsy was consistent with GVHD. No GVHD was observed in the other 9 pts. One pt died of disseminated adenovirus infection early after treatment; viremia was present at the initiation of chemotherapy.
Transient CBU chimerism was detected in 5 of the 10 pts as early as one week and as late as 6 months after CBU infusion. Four pts with median pre-treatment BM blast counts of 56% (range 13-94) had objective hematologic responses (Cheson B JCO 2003) with median post-treatment blast counts of 0% (range 0-12), 3 with morphologic leukemia free state and one with a partial response. One patient had aplastic marrow but with flow cytometry evidence of persistent leukemia; while 4 pts recovered with morphologic persistent leukemia. Six pts went on to receive HSCT. Two subsequently relapsed and one died of disseminated adenovirus, while 3 pts remain in remission.
Conclusion
Use of CBUs as adoptive immunotherapy for pts with refractory myeloid leukemia represents a safe, well tolerated treatment, in which the potential for alloreactivity can be enhanced through the selection of CBUs by targeting shared IPA and NIMA present in the patients. Further, smaller CBUs, unlikely to be adequate grafts for adult transplantation, can be utilized for cell therapy.
Roboz: Cellectis: Research Funding; AbbVie, Agios, Amgen, Amphivena, Array Biopharma Inc., Astex, AstraZeneca, Celator, Celgene, Clovis Oncology, CTI BioPharma, Genoptix, Immune Pharmaceuticals, Janssen Pharmaceuticals, Juno, MedImmune, MEI Pharma, Novartis, Onconova, Pfizer, Roche Pharmace: Consultancy. Ritchie: Celgene: Consultancy, Other: Travel, Speakers Bureau; Pfizer: Consultancy, Other: Research funding to my institution; Incyte: Consultancy, Speakers Bureau; Astellas Pharma: Other: Research funding to my institution; NS Pharma: Other: Research funding to my institution; Bristol-Myers Squibb: Other: Research funding to my institution; Novartis: Consultancy, Other: Research funding to my institution, and travel, Speakers Bureau. Lee: Amgen: Consultancy; Baxalta: Consultancy; Clinipace: Consultancy; Alexion Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal