In this issue of Blood, Lafage-Pochitaloff et al, on behalf of the Group for Research on Adult Acute Lymphoblastic Leukemia (GRAALL), validate the clinical utility of genetics, thereby calling time on treatment strategies that do not incorporate genetic data.1
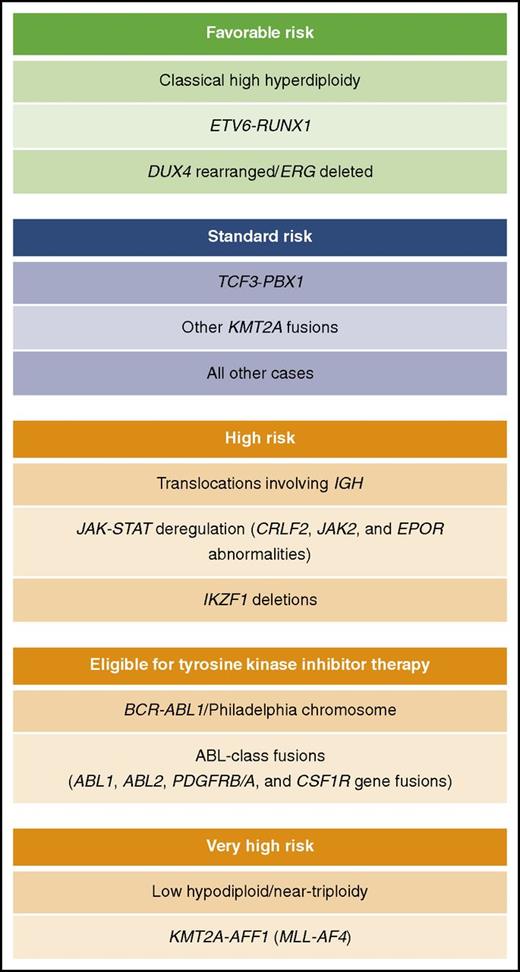
Potential subclassification of B-cell precursor adult ALL by genetics for treatment and risk stratification.
Potential subclassification of B-cell precursor adult ALL by genetics for treatment and risk stratification.
The outcome of adult patients diagnosed with acute lymphoblastic leukemia (ALL) is poor and, with the exception of teenagers and young adults, there has been little improvement in the past few decades.2 In contrast, survival for children with ALL now exceeds 90% for patients treated on contemporary risk-adjusted protocols.3 Virtually all pediatric ALL protocols use genetics and treatment response to direct therapy, whereas the majority of adult protocols are limited to segregating patients on the basis of the presence or absence of the Philadelphia chromosome (Ph), which harbors the BCR-ABL1 fusion gene. Cytogenetic, molecular genetic, and genomic analyses have revealed a heterogeneous genetic landscape in ALL. While there is some overlap in the spectrum of genetic abnormalities underpinning pediatric and adult ALL, the distribution of the lesions is very different.3 The rarity of adult ALL makes compiling large cohorts of patients that have been meaningfully annotated in terms of genetics very challenging.
Using targeted testing and central review, the GRAALL group was able to generate informative genetics on nearly 90% of patients treated on consecutive trials. Overall, their strategy allowed 542 Philadelphia-negative B-cell precursor ALL patients to be classified by both primary and secondary chromosomal abnormalities and the prognostic impact of each one was assessed methodically. This patient cohort is the second largest cytogenetic study of adult ALL, after the United Kingdom ALL XII (UKALLXII)/Eastern Cooperative Oncology Group 2993 (ECOG2993) study4 ; hence, it is an important contribution to the field. The principal finding of this study is that specific primary chromosomal abnormalities are strong and reliable prognostic markers in adult ALL.1 Even though several of the outcome associations have been reported previously, independent validation by a large well-conducted study provides essential evidence for designing risk-stratification algorithms.
A second, and very important, finding was the failure to confirm previous reports suggesting that patients with a complex or monosomal karyotype were associated with a poor outcome.4 Given the subjective nature of these cytogenetic definitions, it is perhaps not surprising that their prognostic impact is less robust than specific abnormalities. Copy-number profiling of complex karyotypes has revealed a heterogeneous profile supporting the notion that these cases do comprise a distinct genetic subtype.5 Recent genomic analyses have revealed a high frequency of the Ph-like ALL subtype among adults.6 Further studies of adult ALL are required to establish whether the specific genetic lesions that underpin Ph-like ALL are prevalent among patients classified as having a complex or monosomal karyotype.
The GRAALL study was also able to examine the prognostic impact of a range secondary chromosomal abnormalities, many of which had been reported, by smaller studies, to be associated with outcome. However, in keeping with the UKALLXII/ECOG2993 study, they found that none of the associations were significant. Secondary chromosomal abnormalities, by definition, are observed in conjunction with primary abnormalities and many, like complex and monosomal karyotype, have somewhat nebulous and subjective definitions. Therefore, their prognostic effect can only truly be assessed within the context of a specific primary chromosomal abnormality. Even within a large cohort such as that compiled by the GRAALL study, this is a challenging exercise. A clear understanding of the prognostic effect of secondary chromosomal abnormalities in adult ALL is only achievable through the retrospective meta-analysis of very large patient cohorts. Although compiling these “mega” cohorts is extremely challenging, especially in rare disease, initiatives such as the HARMONY alliance (www.harmony-alliance.eu) provide excellent opportunities for such studies in the near future.
This GRAALL study was conducted prospectively between 2003 and 2011, and therefore, an understandable shortcoming is the lack of data on the genomic abnormalities that have been described over the past decade. Although several studies have shown IKZF1 deletions to be linked to poor outcome, emerging data suggest that the type of deletion may be an important factor,5,7,8 emphasizing the need for clear definitions and context-dependent analysis. A recent large study by Roberts et al found that patients with Ph-like ALL had a poor outcome compared with the other adults with ALL.6 This observation confirmed a UKALLXII study, which found that patients with CRLF2 deregulation, which underpins approximately one-third of Ph-like ALL, had an increased risk of relapse.5 Importantly, both ABL-class gene fusions and abnormalities that deregulate the JAK-STAT pathway are sensitive to existing targeted therapies (tyrosine kinase and JAK inhibitors, respectively).9 In addition, novel gene rearrangements have been identified in non–Ph-like ALL. For example, a recent study found gene fusions involving DUX4, MEF2D, and ZNF384 in approximately one-third of young adults lacking a classical chromosomal subgroup.10 Although based on limited numbers of patients, initial observations suggest that these lesions may be prognostic. Therefore, genetic characterization of adult ALL can be used not only to risk stratify but also to extend the use of targeted therapy beyond Ph-positive ALL.
The challenge that lies ahead for adult ALL clinicians and researchers is to extend the cytogenetic risk classification established by the GRAALL and UKALLXII/ECOG2993 studies to include additional genetic abnormalities (see figure) and integrate treatment response (as measured by minimal residual disease) to formulate a comprehensive risk algorithm to classify adult ALL.
Conflict-of-interest disclosure: The author declares no competing financial interests.