Abstract

Background: The current management for patients with antiphospholipid syndrome (APS) presenting with arterial thrombosis (AT) remains controversial. There are no prospective data demonstrating the superiority of high over moderate intensity anticoagulation with vitamin K antagonists (VKA) over antiplatelet agents. The Antiphospholipid Antibodies and Stroke Study (APASS showed that the lupus anticoagulant (LA) or anticardiolipin antibodies (aCL) among patients with ischemic stroke did not predict either increased risk for subsequent vascular occlusive events over 2 years or a distinct response to aspirin or VKA. The purpose of our study was to evaluate recurrent thrombosis in patients with APS presenting with AT treated with either antiplatelet and/or anticoagulant therapy.
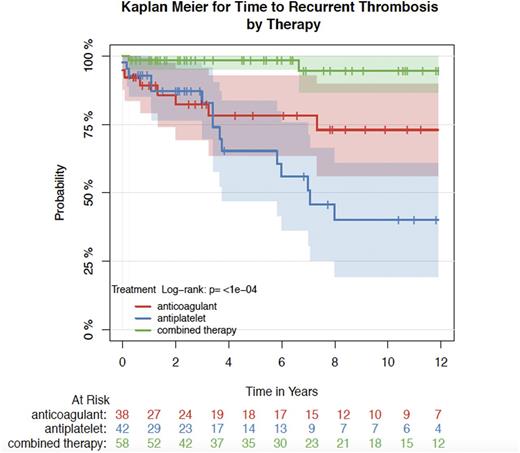
Methods: Using the two antiphospholipid antibody databases (single center [New York Presbyterian Hospital]; and multicenter [APS Alliance for Clinical Trials and International Networking - APS ACTION]), we retrospectively collected the demographic and clinical data of patients with APS who presented with AT. These included gender, age, ethnicity, cardiovascular (CV) risk factors (hypertension, smoking, hyperlipidemia, diabetes and family history of early CV disease), type of antiphospholipid antibodies (aPLs), and treatment modalities (antiplatelet and/or anticoagulant). CV risk factors were only available for patients seen at New York Presbyterian Hospital. The primary outcome was time to thrombosis recurrence and the secondary outcome was any bleeding event while receiving antiplatelet and/or anticoagulant therapy. Kaplan Meier Curves were used to estimate the time at which we expected one fifth of patients to have had a second thrombosis.
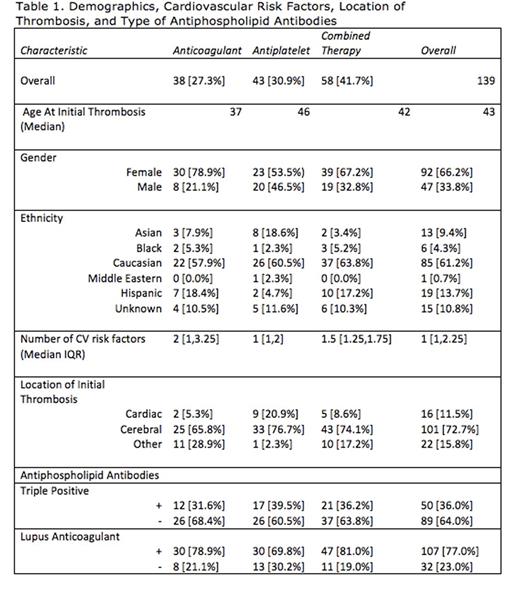
Results: We identified 139 patients, 92 (66.2%) were females. The median age was 42 years (range 18-84). Majority of patients 85 (61.2%) were Caucasian, 19 (13.7%) Hispanic, 13 (9.4%) Asian, 6 (4.3%) Black, and 1 (0.7%) Middle Eastern and the ethnicity of 15 (10.8%) patients were not recorded. Median follow-up time from initial thrombosis was 4.24 years.
Thirty-seven (27.3%) patients were treated with anticoagulants, 43 (30.9%) with antiplatelets, and 58 (41.7%) with both combined. Median age at initial thrombosis was 37, 46, and 42 for the anticoagulant, antiplatelet and combined therapies, respectively. Median number of CV risk factors was 2 in the anticoagulant group, 1 in the antiplatelet group, and 1.5 in the combined therapy group. There were 12 (31.6%), 17 (39.5%) and 21 (36.2%) patients with triple positivity in the anticoagulant, antiplatelet, and combined therapy groups respectively. LA was positive in 30 (78.9%) of patients in the anticoagulant group, 30 (69.8%) in the antiplatelet group, and 47 (81.0%) in the combined therapy group see Table 1. Initial thromboses were observed in cardiac, cerebral, and other arteries. The only major difference across groups was with patients presenting with coronary artery events, who were more likely on antiplatelet agents.
Nine (23.7%) patients in the anticoagulant group, 16 (37.2%) in the antiplatelet group and 4 (6.9%) in the combined therapy group experienced a recurrent thrombotic event. Overall, we estimate that 20% of patients will have had a recurrent thrombotic event within 7.3 years of the initial event. Figure 1
This time varies by treatment, with 7.3, 3.4, and 16.3, years until 20% experience a recurrent event in anticoagulants, antiplatelets, and combined therapy groups, respectively. Compared to those on anticoagulants, patients on antiplatelets have a 2.1-fold increase in the hazard ratio, though due to low power the difference was marginally significant (95% CI 0.90, 4.7, p=0.09). Those on combined therapy had a 70% lower hazard of a recurrent event (HR 0.30, 95% CI (0.08, 0.83, p<0.025).
Bleeding was seen in only one of 26 patients for whom data was available.
Conclusion: Our results suggest that combined antiplatelet and anticoagulation therapy for APS patients presenting with arterial events, compared to antiplatelet or anticoagulant therapy alone, significantly decreases time to thrombosis recurrence and overall recurrence. These results should be confirmed with prospective randomized controlled trials.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal