Abstract
Background: Recent clinical trials of ASCT have demonstrated improved progression-free and overall survival in MM patients. In a population-level analysis, we reported use of ASCT within 12 months of diagnosis was associated with improved overall survival compared to ASCT performed >12 months after diagnosis. Prior studies suggest that non-Hispanic Whites (NHW) were more likely to utilize ASCT than other racial/ethnic groups. However, no population-based studies have considered the effect of race/ethnicity, neighborhood socioeconomic status (nSES) and type of insurance on ASCT utilization.
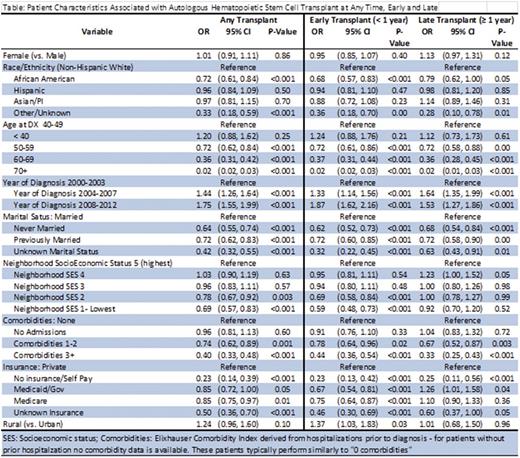
Methods: Patients diagnosed with MM between 2000 and 2012 were identified in the California Cancer Registry linked to the California Patient Discharge Database. Multivariable logistic regression estimated the effect of race/ethnicity, nSES and health insurance on the odds of undergoing ASCT at any time, accounting for age, sex, year of diagnosis, Elixhauser comorbidity index, marital status and urban (vs rural) residence. A multinomial logistic regression was used to determine the effects of covariates on the odds of receiving early (< 1 year from diagnosis) or late (> 1 year) ASCT (vs. no ASCT). Results are presented as adjusted odds ratios (OR) and 95% confidence intervals (CIs).
Results: Of the 14,264 MM cases, 8,084 (57%) were NHW, 2,815 (20%) were Hispanic, 1837 (13%) were African-American (AA), 1326 (9%) were Asian/Pacific Islander (API), and 202 (1%) were of other/unknown race/ethnicity. AA and Hispanics were younger (mean age = 64 for both) than NHW and APIs (mean ages = 68 and 67, respectively). Patients undergoing ASCT were younger than those who did not (mean age 56 vs 69, P<0. 001). The racial/ethnic groups differed by nSES (P<0.001), with higher proportions of NHWs (57%) and APIs (50%) residing in the top 40% of nSES than AAs (30%) and Hispanics (24%). Type of health insurance also varied by race/ethnicity, with Medicaid insurance more common among AAs (13%), Hispanics (16%) and APIs (12%), than NHWs (4.3%), and private insurance more common among NHWs and AAs (49% for both) than Hispanics and APIs (42% for both). Medicare was utilized more frequently by NHW (43%) and APIs (41%) than AAs (34%) and Hispanics (36%) (P<0.001). The proportion of uninsured patients was low overall (1.5%), but somewhat higher in AAs (1.6%), Hispanics (2.9%) and APIs (1.9%) than NHWs (0.9%) (P<0.001).
After accounting for baseline patient characteristics, older age, AA race/ethnicity (vs NHW), increased number of comorbidities prior to diagnosis, being unmarried, diagnosis earlier in the study time-period and lacking health insurance (vs. private) were associated with lower odds of ASCT at any time (Table). The effects of other factors differed for early and late ASCT. Patients residing in rural areas were more likely to receive early, but not late ASCT. Patients who resided in the lowest 2 nSES levels (vs highest nSES level) had lower odds of early, but not late ASCT. While both Medicaid and Medicare were associated with lower odds early ASCT, only Medicaid was associated with an increased use of late ASCT.
Conclusions: This large, population-based analysis indicates that race/ethnicity, neighborhood nSES and insurance status are associated with ASCT use. Lower nSES and Medicaid insurance delayed, but did not prevent, ASCT use, implying that some economic barriers can be overcome. AAs are consistently less likely to undergo ASCT than NHWs, even after adjustment for other predictors, including age, comorbidities, nSES, and health insurance. As AAs are generally diagnosed at younger ages and younger age is associated with increased utilization of ASCT, the nearly 30% decrease in the odds of undergoing ASCT among AAs is striking. Given the demonstrated survival benefits associated with ASCT, further research is necessary to determine and overcome specific barriers to accessing ASCT in patients with MM.
Wun:Janssen Scientific Affairs, LLC: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Daiichi: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal