Abstract

Background: Five large prospective trials have shown a lack of improvement in OS from an autologous-allogeneic (auto-allo) HCT approach in MM, whereas 3 trials have demonstrated benefit. In long term follow up of the randomized EBMT-NMAM2000 trial, Gahrton et al* reported that overall survival (OS) after relapse among the auto-allo cohort was superior compared to auto-auto recipients.
Objective: Compare OS rates after relapse from upfront auto-allo vs. auto-auto HCT. Eligibility: Recipients (N-1679) of either an upfront tandem autologous (n=1110) or auto-allo HCT (n=569) reported to the CIBMTR. Eligibility included age ≤70, planned tandem HCT and recipients of subsequent allo HCT following relapse were excluded. HLA-matched related (96%) and unrelated grafts (4%) were included.
Methods: Cox proportional hazards (PH) regression modeling was used in multivariate analysis of OS after relapse with the clock starting at relapse, and events included death from any cause. Surviving patients were censored at the time of last contact.
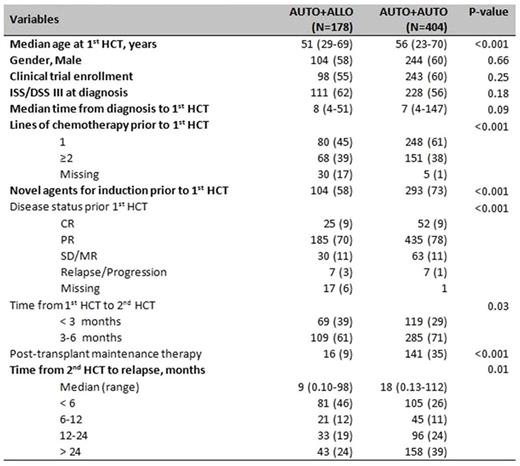
Results/Discussion: 404 patients relapsed in the auto-auto group and 178 patients in the auto-allo group (Table 1). Median time from diagnosis to 1st HCT was 8 months for auto-allo patients and 7 months for auto-auto patient with most patients receiving 1-2 lines of chemotherapy before 1st HCT (73% in auto-allo and 90% in auto-auto groups). Among auto-allo patients, 46% of relapses occurred in < 6 months from 2nd HSCT, compared to 26% in the auto-auto group suggesting that the auto-allo pts were a higher risk group. The median follow-up after relapse for the auto-allo and auto-auto groups were 102 and 99 months respectively.
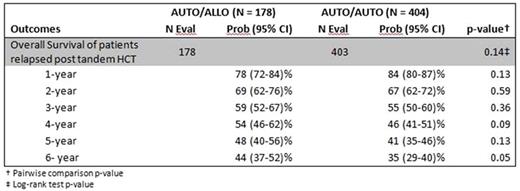
In univariate survival analysis, patients in the auto-allo group had a similar probability of survival (48%) at 5 years post relapse, compared with the auto-auto arm (41%) (Table-2). 101 patients in auto-allo patients died due to MM (69%) vs. 229 (83%) deaths in auto-auto groups due to MM.
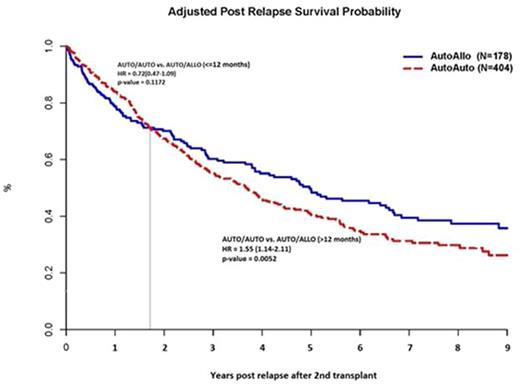
In multivariate analysis, a pattern of differential time dependent risk was observed. Both cohorts had a similar risk of death in the 1st year after relapse (HR of 0.72; p=0.12). However, for time points beyond 12 months after relapse, patients in the auto-allo group had superior OS compared with auto-auto cohort (HR for death in auto-auto =1.55; p=0.0052) (Figure-1). Other significant co-variates associated with superior survival were enrollment in a clinical trial for HCT, male sex and novel agent (lenalidomide/bortezomib) use in induction prior to HCT.
Conclusion: We extend the post relapse survival findings reported by Gahrton et al in allogeneic HCT with matched sibling donors in a larger real world population of related and unrelated grafts. Despite a higher risk population with increased risk of early relapse undergoing tandem auto-allo HCT, we observed a long term reduction in post relapse mortality. This likely reflects an improved response to salvage therapy due to the donor derived immunologic milieu that potentiates the immune effects of agents such as lenalidomide and pomalidomide. With the availability of other agents that modulate immune mediated disease control such a daratumumab (reduction in T and B regulatory subsets) and check point inhibitors; we anticipate that post allo transplant immune manipulation can further augment these benefits.
Patients' Baseline characteristics
* Gahrton et al. EBMT-NMAM2000 study (Blood 2013; 121 (25):5055-63)
Patients' Baseline characteristics
* Gahrton et al. EBMT-NMAM2000 study (Blood 2013; 121 (25):5055-63)
Univariate survival analysis of patients who relapsed post tandem transplant (time 0 at time of relapse)
Univariate survival analysis of patients who relapsed post tandem transplant (time 0 at time of relapse)
Adjusted overall survival for post relapse patients
Krishnan:celgene: Consultancy, Speakers Bureau; takeda: Consultancy, Speakers Bureau; janssen: Consultancy, Speakers Bureau; onyx: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal