Abstract
INTRODUCTION:
Premature vascular disease is a leading cause of late mortality in allogeneic stem cell transplantation (SCT) survivors but the underlying mechanism is not understood. Dyslipidemia is a strong and targetable risk factor for coronary artery disease (CAD) in the general population and its relevance (higher prevalence and high attributable risk in epidemiologic studies of arterial disease) has also been recognized in SCT survivors over the last decade. However, we have previously shown that Framingham risk scores, which rely upon traditional lipid cholesterol measures, are insensitive in determining the presence of CAD. Here, we present the first comprehensive lipoprotein analysis in well-annotated asymptomatic SCT survivors, simultaneously assessed for vascular health using cardiac CT to identify CAD.
PATIENTS & METHODS:
We performed a cross-sectional analysis of 67 survivors who underwent allo-SCT between 1993 and 2012 for hematologic malignancies and survived for at least three years. All subjects received total body irradiation (TBI) based conditioning followed by a 3-4 log ex vivo T cell depleted graft. The median age at transplant was 39 years (range 17-69). The median duration of follow up was 11 years (range 3-22). Sixty percent were male. Seventy percent had some chronic GVHD, but only 23% required immunosuppression at 3 years post transplant. All subjects had a cardiac CT performed and CAD was defined by the presence of either luminal stenosis by angiography or coronary calcification. Cardiovascular clinical data (hypertension, diabetes, dyslipidemia, smoking, CRP, body mass index) and 10- year Framingham risk scores were also collected. Comprehensive lipoprotein analysis was performed on fasting plasma samples using nuclear magnetic resonance (NMR) with the Vantera clinical analyzer (LipoScience Inc., Raleigh, NC). Digitized spectral data signals undergo algorithmic processing to identify and quantify concentrations of lipoproteins and, potentially, small molecule metabolites from a single sample. 13 subjects with history of lipid lowering therapy or absence of plasma sample were excluded. 24 lipoprotein metabolites were measured including particle cholesterol content (_C), particle count (_P), size [small (S_), medium (M_), large (L_), large + medium (LM_)] and average size (_Z). Due to natural variability in the amount of cholesterol per particle, HDL_C/LDL_C and HDL_P/LDL_P levels often are discordant. HDL_P/LDL_P provides a more clinically reliable measure of HDL/LDL quantity than HDL_C/LDL_C.
RESULTS:
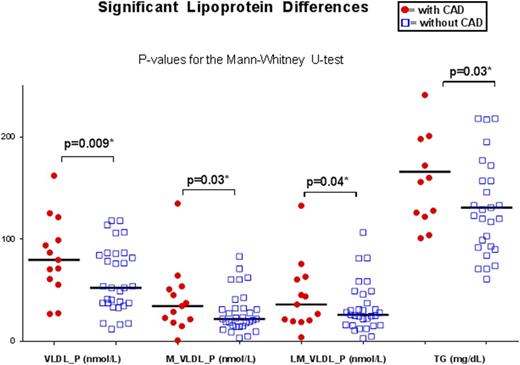
CAD was confirmed in 45% of survivors; 89% of lesions were non-obstructive and 28% of plaques were non-calcified. Lipoprotein analysis on 54 subjects showed no significant association between HDL or LDL particle cholesterol content, particle count or size distribution. Interestingly, measures of Triglyceride and VLDL were significantly higher in survivors with CAD vs no CAD [VLDL_P median 90.4 vs 54.0 nmol/L (p= 0.009), M_VLDL_P 40.2 vs 23.1 nmol/L (p= 0.03), LM_VLDL_P 44.5 vs 26.1 nmol/L (p= 0.04), and total triglycerides (TG) 172 vs 133 mg/dL (p= 0.03)] (Figure 1).
CONCLUSION:
In allo-SCT long term survivors, elevated triglyceride and VLDL counts were associated with early CAD even when traditional targetable measures of dyslipidemia (HDL and LDL) were normal. Future efforts will integrate traditional cardiac risk factors with metabolic markers (lipoproteins, insulin resistance and growth hormone deficiency) to better understand premature coronary artery disease in SCT recipients.
Battiwalla:NIH/NHLBI: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal