Abstract
INTRODUCTION
Acute leukemia (AL) accounts for one third of childhood cancers. Cardiovascular conditions are serious long-term complications of childhood AL. However, few studies have investigated the risk of metabolic syndrome (MetS), a known predictor of cardiovascular disease, in patients treated without hematopoietic stem cell transplantation (HSCT). We describe the overall and age-specific prevalence, and risk factors for MetS and its components in the L.E.A. French cohort of childhood AL survivors treated without HSCT.
METHODS
L.E.A. is a long-term follow-up program involving all childhood AL survivors treated in the French participating centers since 1980 (clinicaltrials.gov identifier: NCT 01756599). MetS was defined according to the National Cholesterol Education Program - Adult Treatment Panel III (NCEP-ATPIII) criteria revised in 2005.
RESULTS
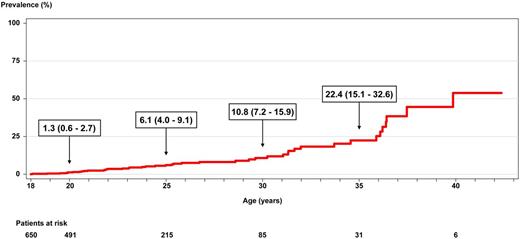
The study included 650 adult patients. The mean age at evaluation was 24.2 years and the mean follow-up after leukemia diagnosis was 16.0 years. Central nervous system (CNS) irradiation was performed in 18.0% of patients (n=117). The prevalence of MetS was 6.9% (95% CI 5.1-9.2). The age-specific cumulative prevalence at 20, 25, 30 and 35 years of age was 1.3%, 6.1%, 10.8% and 22.4%, respectively, as shown in the Figure. The prevalence of decreased HDL-cholesterol, increased triglycerides, increased fasting glucose, increased blood pressure and increased abdominal circumference was 26.8%, 11.7%, 5.8%, 36.7% and 16.7%, respectively.
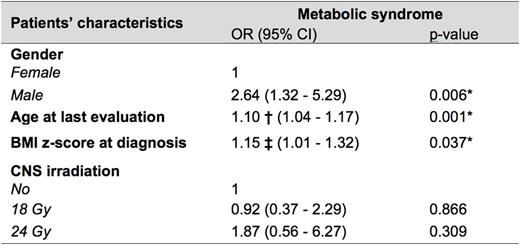
The risk factors significantly associated with metabolic syndrome in the multivariate analysis were male gender, older age at last evaluation and higher body mass index at diagnosis, as shown in the Table. Cumulative steroid dose was not a significant risk factor.
CNS-irradiated and non-irradiated patients exhibited different patterns of metabolic abnormalities, with more frequent abdominal obesity in irradiated patients and more frequent hypertension in non-irradiated patients.
DISCUSSION
Our study aimed to precisely describe the overall and age-specific prevalence, and risk factors of MetS in a large cohort of childhood AL survivors treated without HSCT. Notably, the subgroup treated with chemotherapy alone is one of the largest ever published, which is of particular interest as current protocols include very limited CNS irradiation indications.
The prevalence of MetS was approximately two-fold higher than that observed in the adult French general population under 40 years of age. Moreover, the prevalence of MetS was found to increase markedly with age.
An increased BMI at diagnosis was a risk factor for MetS. Children with an elevated BMI at diagnosis may have a genetic predisposition to metabolic disturbances or a socio-familial environment that renders them more vulnerable to metabolic complications.
CNS irradiation was not found to be a risk factor for MetS. In the literature however, brain irradiation has been frequently reported as a risk factor for MetS. This variation with our study can probably be explained in part by the observation that our irradiated patients displayed a lower risk of elevated blood pressure along with a greater risk of increased abdominal circumference. The irradiated patients may therefore have a different metabolic risk profile compared with the non-irradiated patients, thereby suggesting varying mechanisms of pathogenesis.
The results of our study confirm the need for early and prolonged follow-up of adult survivors of childhood AL even when treated without HSCT and without CNS irradiation. This prerequisite could enable both early detection of metabolic abnormalities and implementation of appropriate therapeutic procedures to reduce the morbidity and mortality associated with cardiovascular complications in such patients.
Multivariate analysis of potential risk factors for the metabolic syndrome
OR: odds ratio; CI: confidence interval; BMI: body mass index; CNS: central nervous system; † OR per each additional year of follow-up; ‡ OR per each additional z-score unit; *significant values (p < 0.05)
Multivariate analysis of potential risk factors for the metabolic syndrome
OR: odds ratio; CI: confidence interval; BMI: body mass index; CNS: central nervous system; † OR per each additional year of follow-up; ‡ OR per each additional z-score unit; *significant values (p < 0.05)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal