Abstract
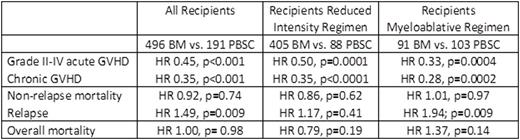
T cell-replete haploidentical donor transplants (HAPLO-HCT) using post-transplant cyclophosphamide for control of alloreactivity is now being increasingly utilized. HAPLO-HCTs were originally performed using BM grafts. However, recently, a few single center studies have reported good outcomes using G-CSF mobilized PBSC grafts for HAPLO-HCT. No prospective randomized comparisons of BM to PBSC grafts for HAPLO-HCT have been performed. Therefore, we analyzed outcomes for 687 adults (496 BM, 191 PBSC) who received HAPLO-HCT for hematologic malignancies using post-transplant cyclophosphamide + mycophenolate + calcineurin inhibitor for GVHD prophylaxis between 2009 and 2014 in the United States. The primary outcome was overall survival. The characteristics of recipients of BM and PBSC were similar except BM recipients were older, more likely to have a performance score ≥90, HCT-CI index ≤2, be CMV seronegative, have a lymphoid malignancy and receive reduced-intensity conditioning. Most PBSC transplants occurred between 2012 and 2014. The median follow-up was 35 and 20 months for recipients of BM and PBSC grafts, respectively. Cox regression models were built to study the effect of graft type adjusted for other significant factors on overall mortality, non-relapse mortality, relapse and graft-versus-host disease (GVHD) and outcomes censored at 2-years to accommodate differential follow-up between treatment groups (Table 1). After adjusting for age, CMV serostatus, disease risk index (disease type/disease status for myeloid and lymphoid malignancy and cytogenetic risk for acute leukemia and myelodysplastic syndrome) and transplant conditioning regimen there were no significant differences in risks for overall mortality (HR 1.00, p= 0.98; 2-year overall survival: 54% and 57%) or non-relapse mortality (HR 0.92, p=0.74; 2-year non-relapse mortality: 17% and 16%) after transplantation of BM compared to PBSC, respectively. However, relapse risks were higher after transplantation of BM compared to PBSC (HR 1.49, p=0.009; 2-year relapse: 45% and 28%). Subset analyses explored the effect of graft type separately for myeloablative and reduced intensity conditioning regimen adjusting for age, CMV serostatus and disease risk index. Consistent with the main analysis there were no differences in overall or non-relapse mortality risks and relapse risks were higher with BM compared to PBSC with myeloablative regimens (Table 1). Although this may in part be explained by lower chronic GVHD risks with transplantation of BM grafts, chronic GVHD was not significantly predictive of relapse risk when modeled as a time-dependent covariate (HR= 0.73, p=0.49). Grade II-IV acute GVHD risks (HR 0.45, p<0.001; 22% and 37%), adjusted for conditioning regimen were lower after transplantation of BM compared to PBSC. Chronic GVHD risks adjusted for age and performance score were also lower after transplantation of BM compared to PBSC (HR 0.35, p<0.001; 20% and 41%) but rates of moderate and severe chronic GVHD were not significantly different (28% and 32%). There were no differences in incidence of hematopoietic recovery by graft type. In conclusion, compared to BM grafts HAPLO-HCT with PBSC are associated with similar overall survival and non-relapse mortality risks but lower relapse risks with myeloablative conditioning regimens. Longer follow up is needed to ascertain whether survival differences may occur later. The observed adverse effect of BM grafts on relapse with myeloablative regimens must be studied further in the setting of carefully controlled trials.
Ciurea:Cyto-Sen Therapeutics: Equity Ownership; Spectrum Pharmaceuticals: Other: Advisory Board. Hamadani:Takeda: Research Funding. Soiffer:Kiadis: Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Juno: Membership on an entity's Board of Directors or advisory committees. Wingard:Ansun: Consultancy; Gilead: Consultancy; Astellas: Consultancy; Fate Therapeutics: Consultancy; Merck: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal