Abstract
Background:Carfilzomib (CFZ) is a novel irreversible proteasome inhibitor (PI) approved for relapsed/refractory multiple myeloma, but its safety and efficacy in AL amyloidosis is not known. We report updated results of an investigator-initiated, multi-center, Phase I/II study of CFZ in AL (NCT01789242), including additional patients (pts) treated in the expansion cohort.
Methods: Eligible pts (relapsed or refractory AL after ≥1 prior therapy; Mayo cardiac stage I or II; LVEF ≥40%; CrCl≥30; CFZ-naive) received CFZ over 30 minutes on days 1, 2, 8, 9, 15, 16 every 28 days, for 8 cycles, given at 20 mg/m2 on days 1, 2 of cycle 1, then at 27, 36, or 45 mg/m2 (depending on cohort) thereafter. Pre-CFZ hydration was recommended during cycle 1, but could be modified or omitted at investigator discretion. Responding pts could continue on a day 1, 2, 15, 16 schedule at investigator discretion. Dexamethasone 20mg with each CFZ dose was added if no VGPR after cycle 4. Primary objectives were safety and determination of MTD. A 3+3 dose escalation design was used, with a planned expansion cohort at MTD. Responses were based on updated AL consensus guidelines. Pts completing ≥2 cycles (or progressing before 2 cycles) were evaluable for response; all treated pts were evaluated for safety. Cardiac function was monitored in all pts by serial NT-proBNP and echocardiograms. Data cutoff was 6/23/16.
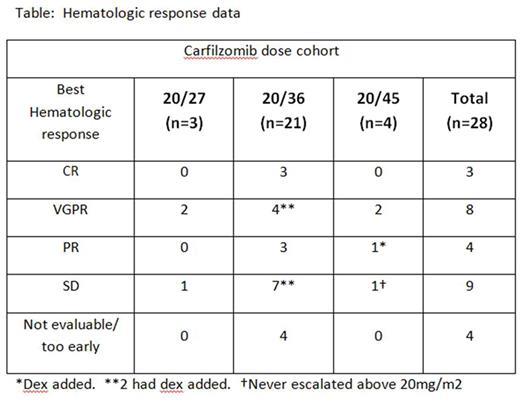
Results: From June 2013 - June 2016, 28 eligible pts were enrolled and treated. Median age was 64 (range 43 - 81); 64% were male. Median time from diagnosis was 31 mos., with median of 2 prior regimens (range 1-5), including bortezomib (96%), IMiDs (43%) and stem cell transplant (46%). Thirteen (46%) were refractory to last therapy, and 10 (36%) were PI-refractory (9 bortezomib, 1 ixazomib). Involved organs included kidney (64%), heart (50%), nerve (25%), GI tract (21%), soft tissue (14%), and liver (11%); 13 pts had ≥2 major organs involved. Median baseline NT-proBNP was 542 pg/ml (range 20 - 13571), and median baseline difference in free light chains (dFLC) was 138 mg/L (range 44 - 4709). There were no DLTs at 20/27 and 20/36 mg/m2. At 20/45 mg/m2, there were 2 first-cycle DLTs of grade 3 fatigue ≥7 days, making 20/36 mg/m2 the MTD. Eighteen more pts have enrolled at MTD. Median number of cycles is 6 (range 1-25+), with 10 pts completing the planned 8 cycles (7 continuing on maintenance), 3 ongoing before cycle 8, and 15 stopping early (9 for AE's, 4 for no response, 2 other). Most common drug-related AE's to date are fatigue (36%), increased creatinine (29%), nausea (25%), dyspnea (18%), anemia (18%), diarrhea (14%), pyrexia, chills, and hypertension (11% each). Grade 3/4 AEs (all-cause) occurred in 20 (71%) pts, including several grade 3/4 cardiac or pulmonary AEs: hypoxia (n=1), lung infection (n=2), chest pain (n=1), hypotension (n=1), hypertension (n=3), decreased ejection fraction/CHF (n=3), and symptomatic ventricular tachycardia (n=2, 1 with cardiac arrest requiring defibrillation). There have been no grade 5 AEs. Of 24 response-evaluable pts, 15 (63%) have responded hematologically (3 CR, 8 VGPR, 4 PR), including 6 of 8 evaluable PI-refractory pts (1 CR, 2 VGPR, 3 PR). Responses have occurred at all dose levels (Table). Dex was added in 5 pts, with 3 response upgrades. Five (21%) pts have had organ responses (3 kidney, 1 GI, 1 liver) to date. With median follow-up of 16 mos. (range 0.5 - 32), 9 pts have had hematologic progression, and 2 have died. To date, 11 pts have had NTproBNP increases of ≥30% and ≥300 pg/ml on CFZ. For 5 this correlated with progressive clinical and/or echocardiographic signs of cardiac dysfunction; the other 6 lacked objective signs of worsening cardiac function, with either no symptoms (n=4) or progressive fatigue (n=2).
Conclusions: CFZ monotherapy is feasible and effective in relapsed/refractory AL amyloidosis, with MTD identified as 20/36 mg/m2 as a 30-minute infusion. Hematologic response rates are promising in this bortezomib-exposed population, including in PI-refractory pts. Cardiac, pulmonary, and renal toxicities were common, warranting close monitoring and dose reductions as appropriate. Similar to IMiDs, NT-proBNP can increase in pts receiving CFZ, without always correlating with progressive cardiac dysfunction, potentially confounding its use as a marker of cardiac response/progression in this setting.
Cohen:Bristol-Meyers Squibb: Consultancy, Research Funding; Janssen: Consultancy. Landau:Spectrum Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees; Prothena: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Onyx/Amgen: Research Funding; Janssen: Consultancy. Scott:Amgen: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees. Kaufman:Novartis: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Pharmacyclics: Consultancy; Incyte: Consultancy. Vesole:Janssen: Speakers Bureau; Novartis: Speakers Bureau; Celgene: Speakers Bureau; Takeda: Speakers Bureau; Amgen: Speakers Bureau. Lentzsch:BMS: Consultancy; Celgene: Consultancy, Honoraria. Gomes:Criterium, Inc: Employment. Comenzo:Karyopharm: Research Funding; Janssen: Consultancy, Research Funding; Prothena: Consultancy, Research Funding; Takeda: Consultancy, Research Funding. Durie:Takeda: Consultancy; Janssen: Consultancy; Amgen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal