Abstract
Background: Patients with a single hematological malignancy (SHM) may be unexpectedly diagnosed with a synchronous dual hematological malignancy (SDHM). Management of such patients is challenging and the impact of therapy on the secondary malignancy is often unknown.
Methods: We reviewed 3036 patients followed in our center from February 2013 to July 2016. Using WHO 2008 criteria we excluded closely-related diseases (e.g. transformed lymphoma, myeloma arising from monoclonal gammopathy of unknown significance (MGUS), lymphoproliferative disorders with associated paraproteins) and included only clonally unrelated SDHMs.
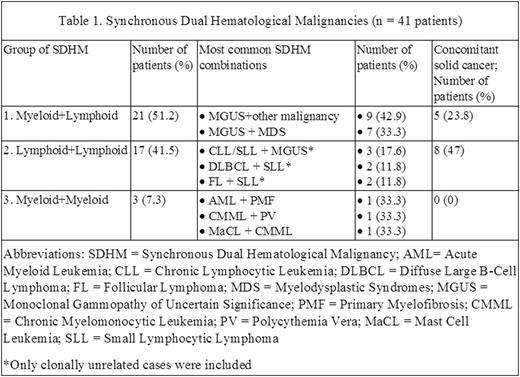
Results: We identified 41 patients with SDHM, a prevalence of 1.35%. Median age was 75 years (range 23-90), with male predominance (26 male, 15 female). All patients were Caucasians except 1 African, and 38/41 were diagnosed locally. Thirteen patients (31.7%) had concomitant solid cancers. Referrals from family practitioners/hospitalists were of two types: 65% with a general diagnosis and 35% with non-specific symptoms requiring work-up. Referrals from specialists (internal medicine or hematology) were more accurate; only asymptomatic secondary diagnoses were missed. SDHMs were diagnosed either incidentally during routine work-up, or because discordant clinical/laboratory findings did not fit a single diagnosis.
Three combinations of SDHMs were identified (Table 1). In the Myeloid+Lymphoid group, concomitant MGUS was most frequent. Within the Lymphoid+Lymphoid group, SDHM combinations were random. There were only 3 Myeloid+Myeloid SDHMs. Twenty-nine patients (70.7%) required initiation of therapy for primary malignancy and 12 (29.3%) were on active surveillance. For secondary diagnosis, 29 (70.7%) patients were actively monitored, and 12 (29.3%) needed treatment (9 simultaneously, 3 delayed). At the completion of treatment for primary malignancy, 37 (90.2%) were either in remission or have non-progressing disease, 4 patients progressed. At the time of data cut-off, 34 patients (82.9%) were alive, compared to 87.2% of patients with SHM. Seven patients died, 3 from disease progression, and 4 from unrelated health issues.
Our management experience of SDHM is following:
- Have low threshold for intensive investigations if there are discordant data
- Patients with low-grade/low-acuity SDHM can be managed safely by active surveillance, with early re-evaluation of both diseases if conditions change
- If two malignancies require treatment, therapy should be aimed at the more aggressive one
- ABVD chemotherapy completely resolved cutaneous T-cell lymphoma lesions
- Cladribine, 6 cycles, had no effect on concomitant chronic myelomonocytic leukemia (CMML)
- Ruxolitinib either precipitated chronic lymphocytic leukemia from B-cell lymphocytosis or accelerated progression
- Hydroxyurea decreased M-spikes in MGUS, regardless of type
- Azacitidine given for CMML positively affected mast cell leukemia and was associated with reduction of bone marrow fibrosis, but had no effect on follicular lymphoma
- Phlebotomized patients with polycythemia vera may develop profound anemia on chemotherapy. We recommend holding phlebotomies and replacing iron stores intravenously. Temporary therapy with erythropoietin-stimulating agents or red cell transfusions may be needed.
Conclusions: SDHMs are not uncommon and require careful investigation if the primary diagnosis is not clear. Myeloid+Lymphoid and Lymphoid+Lymphoid combinations are most common. The high frequency of concomitant solid tumors suggests increased susceptibility to SDHM or impaired immunity. Many second hematological malignancies can be managed by regular monitoring. Active treatment of SDHM requires special considerations. Our recommendations are limited by small patient numbers and a single center. Further studies of SDHM, exploring different cohorts and ethnicities, are needed.
Nay:Gilead Sciences, Inc.: Honoraria; Janssen: Honoraria, Other: Advisory board; Celgene: Honoraria, Other: Advisory board; Amgen: Other: Advisory board; Lyndbeck: Honoraria; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal