Abstract
Introduction: CLL treatment has changed considerably over the last several years, with significant improvement in overall survival and more effective treatment for genetically defined high-risk disease. The physical, intellectual, and emotional challenges of treatment, and living with CLL appear to impact patient quality of life (QOL). We aimed to describe patient distress and perceived impact of having a CLL diagnosis on their well-being using patient-reported CLL risk in a cross-sectional survey.
Methods: From April 2014 to July 2016, the Cancer Support Community (CSC) registered 284 self-identified CLL patients to the Cancer Experience Registry: CLL, an ongoing, online initiative to study the psychosocial impact of CLL. The analysis was limited to US-based registrants diagnosed with CLL who completed survey questions about cancer-related distress (n=134) and perceived impact of CLL (n=99). Twenty-seven items from a validated distress screening tool (α=0.94) were summed for an overall distress score. Four items were summed for a depression score (α=0.85) that was also used to indicate risk for depression (low 0-4 vs. high 5 or greater). Participants were asked to evaluate the perceived impact of CLL on distinct aspects of well-being (QOL, ability to work, life expectancy, relationships, and finances): (1) retrospectively (When you were first diagnosed, how much did you think CLL would affect your well-being?); and (2) at the time of survey response (These days, how much would you say CLL affects your well-being?). CLL risk level (low, intermediate, or high) was captured through patient recall of the doctor's explanation of their estimated risk. We combined low and intermediate risk in analysis.
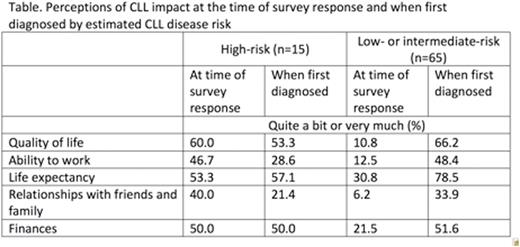
Results: The sample was 53% male and 94% white with median age 62 y and time since CLL diagnosis 6 y. Over half (63%) reported low- or intermediate-risk disease, 17% indicated high-risk, and 20% didn't know their risk. Patients with high-risk CLL (n=20) had significantly higher levels of overall distress (mean=31, SD=23) than patients with low- or intermediate-risk CLL (n=76; mean=21, SD=16, p=0.029). High-risk CLL patients also were more likely to score at high risk for depression (55% vs. 30%; p=0.036). Though overall distress was higher among patients with high-risk CLL, we observed similar top concerns (% moderately to very seriously concerned) for both high- and low- or intermediate-risk groups, respectively: eating and nutrition (56%, 46%); exercising (55%, 34%); worry about the future (50%, 36%); financial worries (50%, 31%); and sleep problems (50%, 30%). Other top concerns among high-risk, but not low- or intermediate-risk patients included ability to think clearly (50%) and feelings of loneliness or isolation (50%). When asked how much CLL currently affects their lives (see Table), high-risk patients (n=15) reported a significantly greater impact on QOL (p<0.001), ability to work (p=0.002), relationships with friends and family (p=0.002), and finances (p=0.029) than low- or intermediate-risk patients (n=65). Interestingly, when asked to recall how much they thought CLL would affect their lives when first diagnosed, there was no difference in anticipated impact between those with low- or intermediate-risk and high-risk patients. And in both risk groups, 83% indicated they understood how lab test results reflected their risk.
Conclusion: These initial data from our CLL registry suggest that most patients understand their estimated risk and that high-risk CLL patients experienced greater overall distress and depression risk at the time of survey response compared to patients with low- or intermediate-risk. Across disease risk categories, CLL patients anticipated considerable distress (see Table) when first diagnosed and reported similar top concerns. These findings can help clinicians shape discussions that are responsive to CLL patient and care partner concerns about diagnosis, treatment and survival.
Flowers:AbbVie: Research Funding; TG Therapeutics: Research Funding; Gilead: Consultancy, Research Funding; NIH: Research Funding; Mayo Clinic: Research Funding; Roche: Consultancy, Research Funding; Millenium/Takeda: Research Funding; Pharmacyclics, LLC, an AbbVie Company: Research Funding; Infinity: Research Funding; ECOG: Research Funding; Acerta: Research Funding; Genentech: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal