Abstract
Introduction:
Data are limited on the use of hospice services for diffuse large B cell Lymphoma (DLBCL). As DLBCL is treated in both academic and community settings, there may be variations in hospice enrollment due to both patient and practitioner characteristics. We aimed to identify predictors for hospice enrollment for DLBCL patients, and to compare total costs of care and components of cost among hospice and non-hospice DLBCL patients in the 30 days prior to death.
Methods:
Using the SEER-Medicare database from 2002-2012, we identified DLBCL patients 65 years and older using ICD-O3 codes. Patients were excluded if they did not die, died within 30 days of diagnosis, or had a secondary cancer diagnosis. We investigated predictors of hospice enrollment within the last 30 days of life including sex, race, age, marital status, residence, modified Charlson Comorbidity Index (CCI), income, time from diagnosis to death, practice type, region, and chemotherapy use. Using generalized estimating equation using a log link and gamma distribution, we evaluated adjusted and unadjusted costs for the last 30 days of care, aggregated into 5-day periods among hospice and non-hospice users, separating costs into inpatient, outpatient, hospice, office visits, and diagnostic testing. We tested the robustness of our finding using a time-varying propensity score weighted model.
Results:
We identified 12,644 DLBCL patients. Hospice users were older than non-users (mean age: 80 vs. 78 years, p<0.001), more often white (92.9 vs 91%, p=0.02), less likely to be married (45.1 vs 53.7, p<0.001) and were more likely to be female (61.2% vs. 52.1%, p<0.001). Patients diagnosed at stage 1 were less likely to enroll in hospice than those with more advanced stage (26.7 vs. 30.9, p=0.004). There were no significant differences in enrollment by urbanicity, neighborhood poverty level, and CCI. Non-hospice patients were more likely than hospice users to have received transfusions (p<0.001) and chemotherapy (p<0.001) in the last 30 days of life. There was no difference in proportion being treated in academic vs community settings for hospice and non-hospice users.
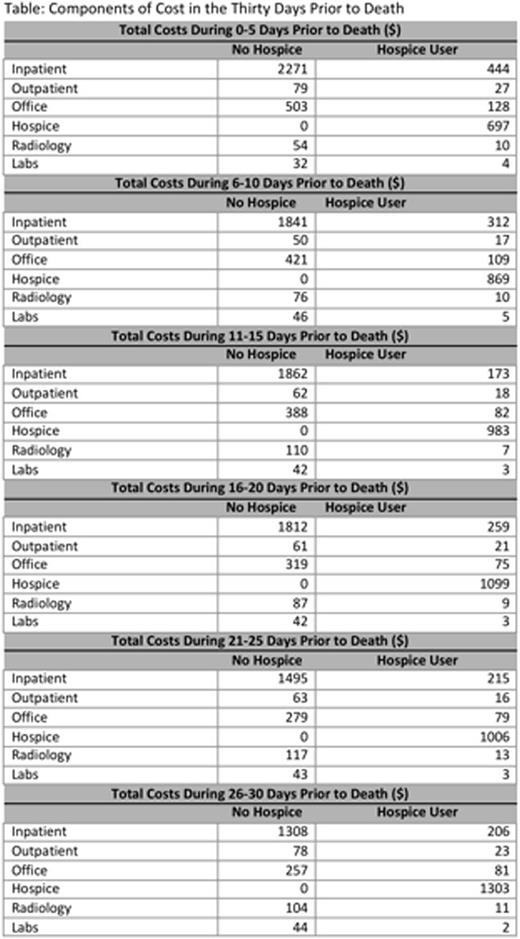
In the last 30 days prior to death, we found that costs continually increased for non-hospice users from $2,063 for days 26-30 prior to death to $3,068 for the last five days of life (p<0.001). However, hospice users' costs decreased over this time period from $1,752 to $1,326 (p=0.002) (Figure). Our results were consistent after adjusting for age, CCI, Ann Arbor stage, race, marital status, urbanicity, and census tract poverty level ($2,041 days 26-30 vs. $3,109 days 0-5 for non-hospice users, p<0.001; $1,800 days 26-30 vs. $1,348 days 0-5 for non-hospice users, p=0.001). For non-hospice patients, inpatient admissions drove costs ($2,289) and for hospice patients, hospice costs drove costs ($443). Non-hospice users had higher costs in all categories of care (Table). Our propensity score weighted models provided similar results.
Conclusion:
Using data from SEER-Medicare, we found differences in patient characteristics associated with hospice use among older adults with DLBCL, specifically age, race, marital status, and sex. Those who received transfusions or chemotherapy in the last 30 days of life were less likely to enroll in hospice. Community vs. academic settings was not associated with hospice enrollment. We also identified differences in healthcare utilization in the last 30 days of life among hospice and non-hospice patients. Total health care costs were significantly higher over the last 30 days of life in non-hospice patients, and the primary cost driver is inpatient admissions. Further analyses will help to identify those patients who did not receive hospice services, but received palliative care. Earlier hospice intervention may reduce costs of care for older patients with DLBCL in the last 30 days of life.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal