Abstract
Introduction: Approximately 27,000 new cases of multiple myeloma (MM) are diagnosed in the United States each year, and over 11,000 deaths annually are attributed to MM (http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-044552.pdf). In the past decade, the introduction of new drugs has markedly changed the treatment paradigm and outcomes for patients with MM (Kumar et al. Leukemia 2014;28:1122-1128). However, it is not clear whether the improvements have been sustained in more recent years and if improvements were also experienced by patients with additional risk factors for death. This study examined temporal changes in MM survival among patients with additional factors known to be associated with death (i.e. older age and cardiac conditions).
Methods: This was a retrospective observational cohort study using the Truven Health MarketScan® Commercial and Medicare Supplemental Databases. Study patients included those with at least 1 inpatient or 2 outpatient claims with an MM diagnosis between January 1, 2006 and December 31, 2014, who were at least 18 years old at diagnosis, were continuously enrolled in a health plan for at least 12 months before and at least 30 days after the first diagnosis, and had no prior history of any malignancies. Patients were followed from the date of the first MM diagnosis through the earliest event including death, end of enrollment, or end of the study period (September 30, 2015). All-cause mortality data were obtained from inpatient admissions with a discharge status of "death," and from Social Security Administration death records. Mortality rates were calculated overall, for patients <65 years-old and ≥65 years-old, and for patients with and without a cardiac comorbidity (heart failure, dysrhythmia, myocardial infarction, other ischemic heart disease) indicated in the 12-month baseline period grouped within two time periods according to the date of MM diagnosis (2006-2010 and 2011-2014). Kaplan-Meier survival curves were created for each group and compared using log-rank tests.
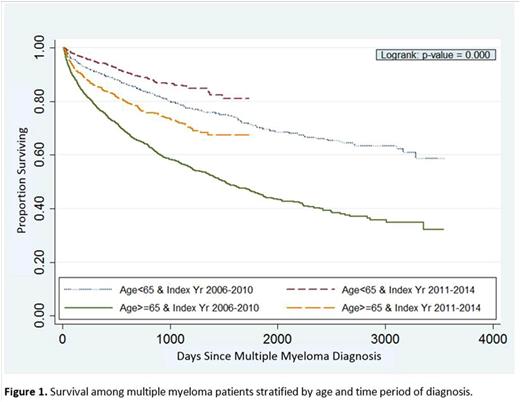
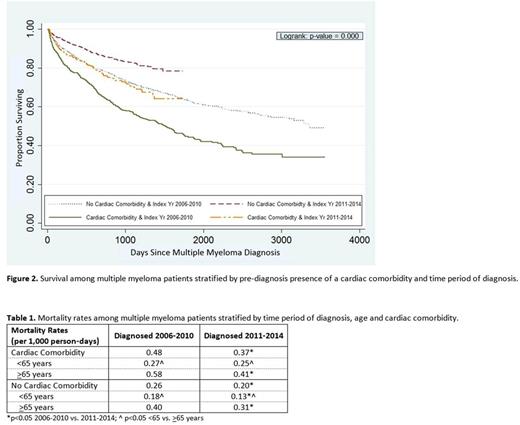
Results: A total of 5,199 MM patients met all eligibility criteria and were included in the analysis. There were significant differences in survival between patients stratified by age and time period of diagnosis (Figure 1). The overall mortality rate was substantially lower among all patients <65 years-old, compared to those ≥65 (0.18 vs. 0.43 per 1,000 person-days, p<0.05), and mortality rates improved among both age groups from the 2006-2010 to the 2011-2014 time period (<65 years: 0.19 vs. 0.15 per 1,000 person-days, p<0.05; ≥65 years: 0.47 vs. 0.35 per 1,000 person-days, p<0.05). Over 41% of MM patients ≥65 years-old had a cardiac comorbidity, compared to approximately 17% of those <65 years-old. There were significant differences in survival between patients stratified by the presence of a cardiac comorbidity and time period of diagnosis (Figure 2). The mortality rates improved from the 2006-2010 to the 2011-2014 time period among both groups (no cardiac comorbidity: 0.26 vs. 0.20 per 1,000 person-days, p<0.05; cardiac comorbidity: 0.48 vs. 0.37 per 1,000 person-days, p<0.05) (Table 1). Patients who were ≥65 and with a cardiac comorbidity had the worst survival in both time periods; however, mortality rates improved from the 2006-2010 to 2011-2014 time period for all groups stratified by age and presence of a cardiac comorbidity (Table 1).
Conclusion: This real-world analysis showed improved survival over time in patients with MM. Improvements in survival were most pronounced for older patients with a cardiac comorbidity, suggesting that changes in disease management over time may have contributed to better outcomes even among the most vulnerable MM patients. With the recent FDA approval of new MM treatment options, tailoring treatment plans for patients based on specific risk factors is even more feasible and may help to further optimize disease management and continue the improvements in survival.
Maiese:Janssen Scientific Affairs, LLC: Employment. Evans:Truven Health Analytics: Employment. Irwin:Truven Health Analytics: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal