Abstract
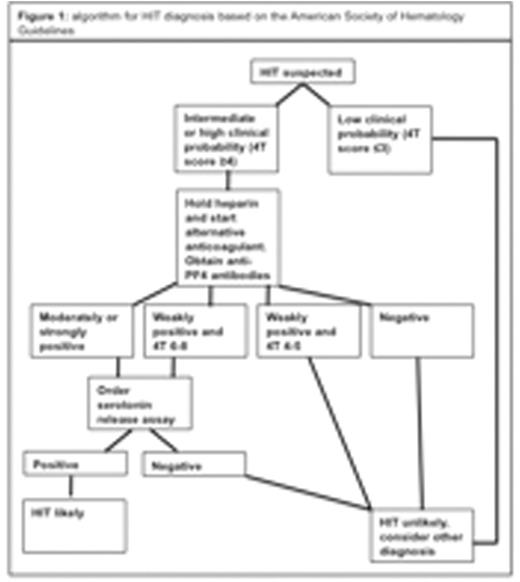
Introduction:Thrombocytopenia is a common problem in hospitalized patients, which has a diverse etiology. One of the infrequent causes is heparin-induced thrombocytopenia (HIT), a complex immune disorder in which heparin leads to the production of IgG antibodies, targeting platelet factor 4 (PF4). HIT diagnosis is based on a decrease in the platelet count of more than 50% beginning 5 to 10 days after starting heparin, in association with platelet-activating HIT antibodies (screening test), positive functional tests (confirmatory tests), in patients with no alternative causes for thrombocytopenia, necrosis or thrombosis (Figure 1).
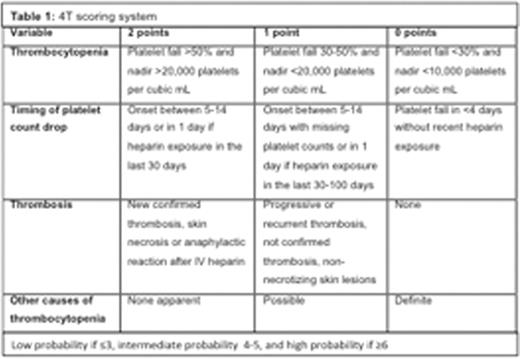
Most patients admitted to our institution receive unfractionated or low molecular weight heparin for venous thromboembolism prophylaxis. The risk of HIT depends on the type of heparin the patient receives. Even though HIT is rare, we tend to have a high suspicion and low threshold to order laboratory workup for this condition, occasionally without using the 4T«s score (Table 1). The 4T«s score is a validated system with a very high negative predictive value (NPV) of up to 99%, when the score is ²3. The aim of this study is to determine if the 4T«s score has been used appropriately in our institution. It is a very useful tool with a high negative likelihood ratio and using it systematically may decrease unnecessary laboratory testing, consequently decreasing costs and potentially length of stay.
Methods:This is a retrospective descriptive study from a single teaching community hospital. Between January and December of 2015, 57 HIT screening tests (PF4 ELISA) were ordered in our institution. We reviewed all of the patient charts to determine their 4T«s score. The patients were divided into low, moderate and high pretest probability based on their score (low probability if ²3, intermediate 4-5, and high if ³6). The data analysis was completed with SPSS software.
Results:57 tests were ordered, 5 patient charts did not have enough information to calculate 4T«s score and were excluded. 52 charts were reviewed, 28 patients were male and 24 were female (53 and 46% respectively), and they were between 25 and 89 years of age. 7 (13.4%) did not receive heparin (during current hospitalization or within 100 days), 11 (21.1%) received therapeutic doses of unfractionated heparin, 11 (21.1%) received prophylactic doses of unfractionated heparin, and 23 (44.2%) received prophylactic low molecular weight heparin (enoxaparin). The 4T«s score was calculated for each patient; 40 were low risk, 10 intermediate risk and 2 high risk (76.9, 19.2, 3.8% respectively). All the patients had HIT screening antibodies ordered; only 10 (19.2%) were positive and from those only 1 (1.9%) was confirmed by the serotonin release assay. This confirmed patient had a 4T«s score of 6. Of the 7 tested patients who did not receive heparin, none had a positive screening test (all had 4T«s score of 1 or 2). 35 of the screening tests were ordered by internal medicine residents, 5 by surgical residents, 12 by attending physicians (67.3, 9.6 and 23% respectively).
Previous studies validated that a 4T«s score of ²3 can predict negative results for the confirmatory tests. By using theMcNemar«stest for matched pairs, we attempted to determine a cut off for the 4T«s score that would predict a negativeHIT screeningtest. We found that a 4T«s score ²2 predicted a negativeHIT screeningtest, with aNPVof 75% (p=0.0018). Since our study included a small patient cohort and due to the possibility of laboratory work up not being ordered in patients with a low 4T«s score, we suspect theNPVis actually lower than our current finding. A prospective study with a larger cohort of patients would be necessary to confirm these findings.
Conclusions:Only 12% of the patients had a 4T«s score ³4 that would warrant laboratory work up, therefore we concluded that PF4 ELISA screening tests have been over utilized in our institution, increasing false positive results, length of stay and cost of hospitalization in patients without a significant risk for HIT. This could be avoided by calculating the 4T«s score before obtaining any further laboratory tests. The 4T«s scoring system has been validated by multiple studies with large cohorts in the past. We will continue to work with our staff, especially the residents, to improve education on HIT and adequate diagnosis, based on current guidelines.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal