Abstract
Second allogeneic hematopoietic cell transplant (HCT) may be indicated for relapsed hematological malignancies or graft failure. However, there are limited data in the literature concerning outcome post second allogeneic HCT. The purpose of the presented study was to investigate parameters that may influence outcome post second allogeneic HCT.
This single centre retrospective study at the Princess Margaret Cancer Centre examined 92 patients that underwent second HCT from 1980-2015. First HCT was done for patients with median age 35 years (range 9-68), for various hematological diseases (AML 26 patients, CML 28 patients, aplastic anemia 14 patients, ALL 11 patients, other diseases 13 patients). Donors were related for 78 patients (85%) versus unrelated for 14 (15%). Graft was bone marrow for 71 patients (77%) versus peripheral blood stem cells (PBSC) for 21 (23%).
For the second HCT, median age was 40 years (range 16-69, age ≤40 n=46, >40 n=46). The indication for second HCT was either relapsed hematologic malignancy for 59 patients (64%, 12 patients relapsed ≤6 months post first HCT), versus graft failure for 33 patients (36%). The median time from first HCT until relapse or graft failure was 11 months (1-206 months). The median time from first HCT until second HCT was 18 months (range 1-212). Year second HCT was performed was grouped into 1980-1995 (n=28), 1996-2005 (n=42), 2006-2015 (n= 22). Fifty-two patients (57%) had ECOG 0-1 versus 40 patients (43%) with ECOG 2-3. Preparative regimen was myeloablative (MA) for 47 (51%) versus 45 with other regimens (49%). Calcineurin inhibitor-based GVHD prophylaxis was used in 75 patients (82%). Eighty-three patients (90%) used the same donor versus only 9 patients (10%) which had a different donor. The type of graft at second HCT was PBSC in 54 patients (59%) versus BM for 38 patients (41%). Among the 82 patients with count recovery data, median neutrophil count ≥0.5/µL was 18 days (range 8-54), and platelet recovery ≥20/µL was 16 days (range 10-88). Among the 66 patients that died, cause of death was relapse in 17 patients (26%), infection in 18 patients (27%), GVHD in 6 patients (9%), graft failure in 6 patients (9%) and other complications in 19 patients (29%).
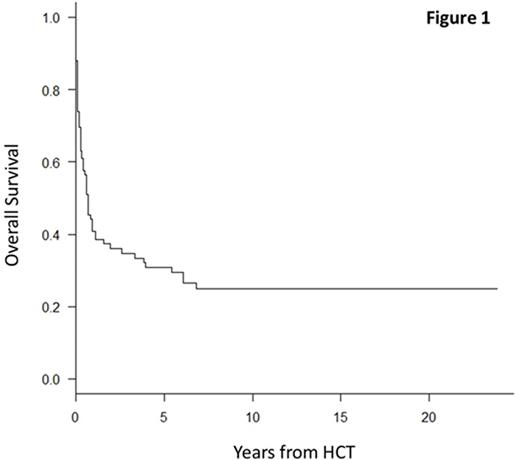
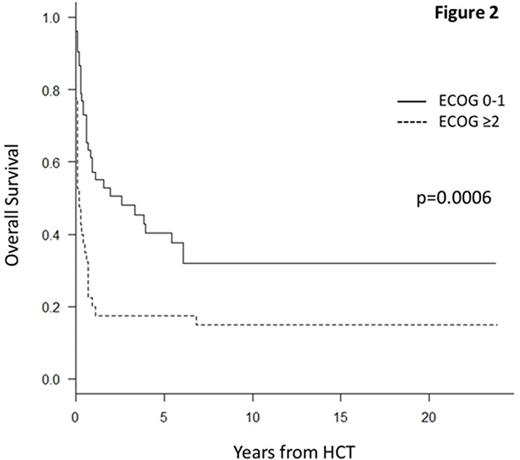
Median follow up of survivors was 120 months (range 5-286). Three-year overall survival (OS) of the entire cohort was 35% (95% CI=25-45) (Figure 1). Univariate analysis for OS examined second HCT indication (3-year OS 43% for relapse versus 20% for graft failure, p=0.02), ECOG score (3-year OS 48% for ECOG 0-1 versus 18% for ECOG ≥2, p=0.0006, Figure 2), time from first HCT to relapse/graft failure (3-year OS for <12 months 21% versus ≥12 months 46%, p=0.009), preparative regimens (3-year OS for MA 42% versus other regimens 23%, p=0.08). Age at second HCT (≤40 versus >40 years, p=0.2), time period second HCT was performed (p=0.7), use of different donor (p=0.3) and graft source for second HCT (p=1.0) were not significant.
Multivariable analysis for OS demonstrated ECOG score at second HCT (HR=2.15 for ECOG ≥2, 95% CI=1.32-3.51, p=0.002) and indication for second HCT (HR=1.67 for graft failure, 95%CI=1.02-2.75, p=0.04) to be the only independent prognostic variables influencing survival in this cohort. In conclusion, second HCT may provide prolonged survival, particularly for patients transplanted for relapsed disease following first HCT, and with a favorable performance status.
Lipton:Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Ariad: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal