Abstract
Introduction: Autologous stem cell transplantation (ASCT) is currently considered the standard first-line consolidation therapy for younger patients with mantle cell lymphoma (MCL). In general, there are limited data regarding a preferred high-dose therapy (HDT) regimen preceding ASCT to be used in patients with non-Hodgkin lymphoma (NHL). Although BEAM and BEAC regimens (including BCNU, etoposide, cytosar in both regimens and melphalan or cytoxan, respectively) have been commonly employed as conditioning HDT in patients with aggressive or recurrent NHL, there have been few reports comparing these two regimens. A retrospective analysis found the superiority of BEAM over BEAC in terms of overall survival (OS) and event-free survival (EFS). Regimen-related toxicities were similar, except that BEAM was associated with more frequent lower gastrointestinal mucositis. Other studies reported that these two regimens had equivalent efficacy and outcome, as measured by EFS and OS. Further studies are required to define the optimal regimen for each specific NHL subtype. The current study aimed to compare the efficacy and toxicity of BEAC versus BEAM as a consolidation HDT in young patients with MCL undergoing ASCT.
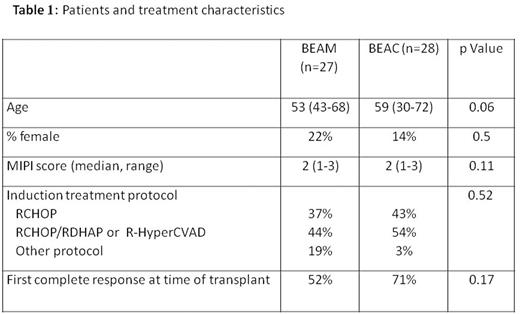
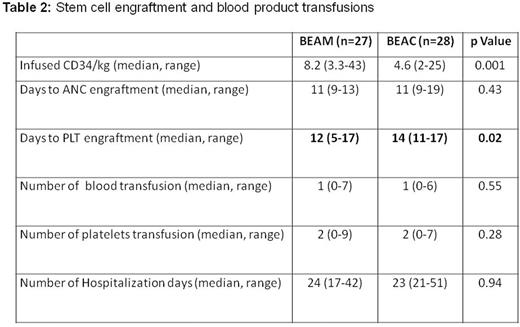
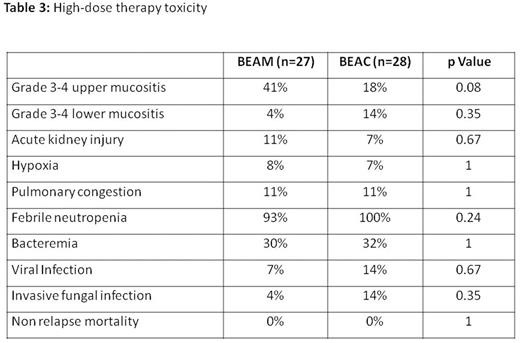
Methods: This is a retrospective analysis of outcomes in patients with MCL who received high-dose chemotherapy with BEAM or BEAC regimen followed by ASCT in two bone marrow transplant centers in Israel. OS, progression-free-survival (PFS) and regimen toxicity were compared. Results: Fifty five patients with MCL who were diagnosed between 1995-1/2016 and received consolidation with BEAC or BEAM HDT regimen were included in the analysis. Twenty seven patients were treated with BEAM and 28 patients - with BEAC. No significant differences between the two groups were revealed in terms of age, sex, the Mantle Cell Lymphoma International Prognostic Index (MIPI), induction treatment protocol and percentage of patients who were transplanted at first complete response (CR1) (Table 1). The amount of infused CD34 cells was significantly higher in the BEAM group, and the number of days until platelet engraftment was significantly greater in the BEAC group. There were no differences in the number of blood transfusions or hospitalization days between the groups (Table 2). In terms of HDT toxicity, there was a trend to a higher rate of grade 3-4 upper mucositis with BEAM protocol; no other differences in toxicity between the regimens were observed (Table 3). Non-relapse mortality at day 30 post-transplant was 0% in both groups. A median follow-up of surviving patients was 31 (range 1-119) months. PFS at 3 years in patients receiving BEAM and BEAC was 65% and 78%, respectively (p=.75). In univariate analysis, age less than 60 years, low-to-intermediate MIPI and transplant at CR1 were found to significantly improve PFS, while no difference in PFS was found between the two treatment regimens. In multivariate analysis, low-to-intermediate MIPI and transplant at CR1 appeared to significantly increase PFS (P = 0.02 and 0.03, respectively). There was no difference in the 3-year OS between the two HDT regimens (58% in the BEAM group and 81% in the BEAC groups; p=.31). Conclusion: BEAC and BEAM high dose chemotherapy regimens followed by autologous stem cell transplantation have similar efficacy and toxicity in patients with MCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal