Abstract
Introduction Auto-SCT, still remains as the standard therapy for patients with MM deemed to be eligible for this approach. Unfortunately, even when most patients will respond to auto-SCT, 10-20% of cases will progress within a year. Over the last few years, a dramatic improvement on clinical outcomes has been made by using novel agents in the treatment of MM. Based on the above mentioned, we aimed to assess the incidence of Early Relapse (ER) for patients undergoing auto-SCT treated with novel-agents induction combinations at our center and to explore possible predictor factors.
Methods All consecutive patients who underwent single auto-SCT at Tom Baker Cancer Center (TBCC) from 01/2006 to March/2016 were evaluated. ER was defined as per recent publications (<12 months from auto-SCT). Two-sided Fisher exact test was used to test for differences between categorical variables. A p value of <0.05 was considered significant. Survival curves were constructed according to the Kaplan-Meier method and compared using the log rank test. All statistical analyses were performed by using the SPSS 24.0 software.
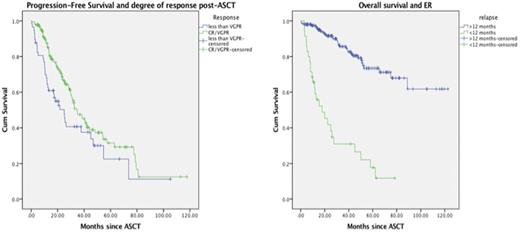
Results 232 consecutive patients with MM underwent single auto-SCT at our Institution over the defined period. Clinical characteristics are shown in Table 1. At the time of analysis, 172 patients are still alive and 112 have already progressed. Among these cases, 35 patients have relapsed in <12 months (ER) from auto-SCT (15.1%). 16 out of 35 patients with ER had HRC (high-risk cytogenetics) (45.7%). ER was seen in 25% of cases with HRC and 11% of patients with Standard Risk (SRC) (p=0.01). Patient with <VGPR at day-100 post-ASCT exhibited a shorther PFS (24 months vs 34 months, p=0.03) (Fig1b). Patients with <VGPR at day-100 post-ASCT were more likely to develop ER (31.5% vs 9%). (p=0.001) The use of lenalidomide maintenance or any consolidation strategy did not impact on the rate of ER (p=0.1 and 0.4, respectively). Neither the type of conditioning regimen nor the induction chemotherapy (p>0.5) was associated to a higher rate of ER. Median OS was shorter for the ER group (17.8 months) compared to an estimated 93 months for those patients relapsing >12 months. (p=0.0001)
In conclusion, patients with ER after auto-SCT remain to be a challenge. Even with the advent of novel agents, patients with ER had poor outcomes. ER seems to be associated to HRC and low degree of response. Patients with these features should be considered for novel alternatives, aiming to achieve and sustain the deepest possible response. More biological insights on ER cases are needed to further improve survival outcomes.
PFS according to level of response at day-100 post ASCT
Overall survival according to the pattern of relapse
Jimenez-Zepeda:Amgen: Honoraria; Takeda: Honoraria; Janssen: Honoraria; Celgene, Janssen, Amgen, Onyx: Honoraria. Neri:Celgene and Jannsen: Consultancy, Honoraria. Bahlis:Onyx: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Other: Travel Expenses, Research Funding, Speakers Bureau; Janssen: Consultancy, Honoraria, Other: Travel Expenses, Research Funding, Speakers Bureau; BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal