Abstract
Background: Because of the disruption of BCNU (Carmustine) in France during several months, and based on the results reported by Visani and colleagues (Visaniet al, Blood 2011) Bendamustine has been used in combination with Etoposide, Cytarabine and Melphalan (BeEAM) in a new high dose conditioning regimen before autologous transplant in relapsed/refractory (R/R) lymphoma patients. We report our experience on the safety and efficacy of BeEAM compared to the classical BEAM regimen.
Patients and methods: Ninety consecutive pts (BEAM = 60, BeEAM = 30) with R/R lymphoma were enrolled between December 2013 and September 2015 (BEAM from December 2013 to January 2015 and BeEAM from February to September 2015) in this retrospective study. Pts in complete or partial response after salvage therapy received high dose conditioning with Bendamustine (d-8 and d-7), Cytarabine (400 mg/m2 continuous infusion from d-6 to d-3), Etoposide (200 mg/m2 continuous infusion from d-6 to d-3) and Melphalan (200 mg/m2 d-2) followed by ASCT on d0. Bendamustine was given at 200 mg/m2/d for the first 4pts then 100 mg/m2/d for the 4 subsequentpts and finally at 120 mg/m2/d for the remaining pts (22 pts). Among the BEAM group, 68% had Non-Hodgkin's Lymphoma (NHL) and 32% Hodgkin's Lymphoma (HL) compared to 87% and 13% respectively in the BeEAM group (p = 0,014). HHV-6 detection was performed by PCR for symptomatic pts (fever, rash or prolonged cytopenia). Patients were housed in single bedrooms with air filtration and received the same supportive care.
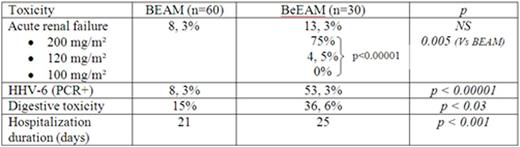
Results: Median age was 50 (18-66) and 56 (20-67) in the BEAM and BeEAM groups respectively and median of previous chemotherapy regimens was 2 (1-5). Fifty two out of 90 patients were male (37/60 in the BEAM group and 15/30 in the BeEAM group). Pts were in CR (46, 7% Vs 56, 7%) or PR (53, 3% Vs 43, 3%) at time of transplant. There was no difference in terms of hematologic recovery (median = 11 days (range: 7-22)), blood and platelets transfusion, mucositis toxicity. There was no statistical difference in the incidence of acute renal failure when comparing the two groups. However, there was a very striking difference when considering the highest dose of Bendamustine when compared as well to the two others doses of Bendamustine (p < 0.00001) as to the BEAM group (p=0.005). Additionally, we also observed a high incidence of symptomatic HHV-6 infections (53.3% vs 8.3%, p < 0.00001), digestive toxicity (36.6% vs 15%, p = 0.03) and a longer hospitalization duration (25 days (range: 18-59) vs 21 days (range: 18-32), p = 0.001) for patients in the BeEAM group overall.
With a median follow up of 18.3 and 9.7 months for BEAM and BeEAM respectively, overall survival (93% vs 86%), transplant related mortality (0% vs 3%) and event free survival (83% vs 78%) were comparable.
Conclusion: Overall, BeEAM regimen was associated with longer duration of hospitalization, higher rate of digestive toxicity and increased risk of symptomatic HHV-6 infection as compared to the BEAM regimen. In addition, higher doses of Bendamustine (200mg/m2/d for two consecutive days) were associated with unacceptable high rate of acute renal toxicity. With a still short follow-up, the absence of benefit on disease control together with higher short term toxicity does not allow to recommend the use of BeAM instead of classical BEAM. Should it be used, we suggest that pts should be carefully monitored for renal toxicity and for HHV-6 infection in case of symptoms.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal